SLAP Tears
A SLAP tear is an injury to the labrum of the shoulder, which is the ring of cartilage that surrounds the socket of the shoulder joint.
Anatomy
Your shoulder is a ball-and-socket joint made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
The head of your upper arm bone fits into a rounded socket in your shoulder blade. This socket is called the glenoid. Surrounding the outside edge of the glenoid is a rim of strong, fibrous tissue called the labrum. The labrum helps to deepen the socket and stabilize the shoulder joint. It also serves as an attachment point for many of the ligaments of the shoulder, as well as one of the tendons from the biceps muscle in the arm.
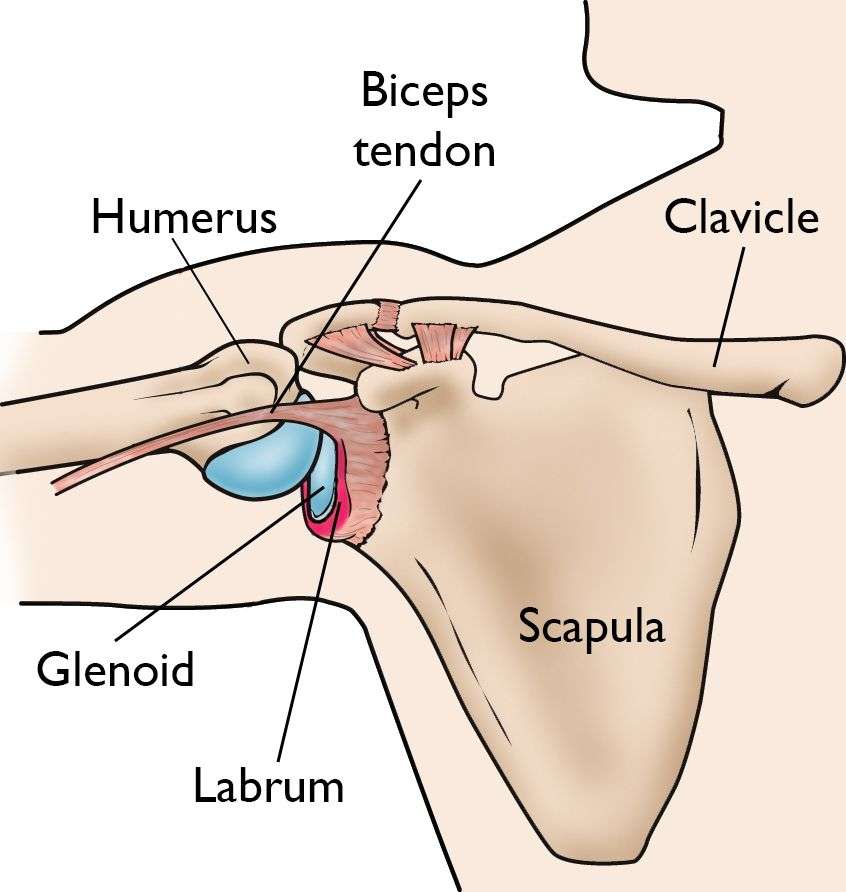
The labrum deepens the socket of the shoulder joint, making it a stronger fit for the head of the humerus.
Description
The term SLAP stands for Superior Labrum Anterior and Posterior. In a SLAP injury, the top (superior) part of the labrum is injured. This top area is also where the biceps tendon attaches to the labrum. A SLAP tear occurs both in front (anterior) and back (posterior) of this attachment point. The biceps tendon can be involved in the injury, as well.
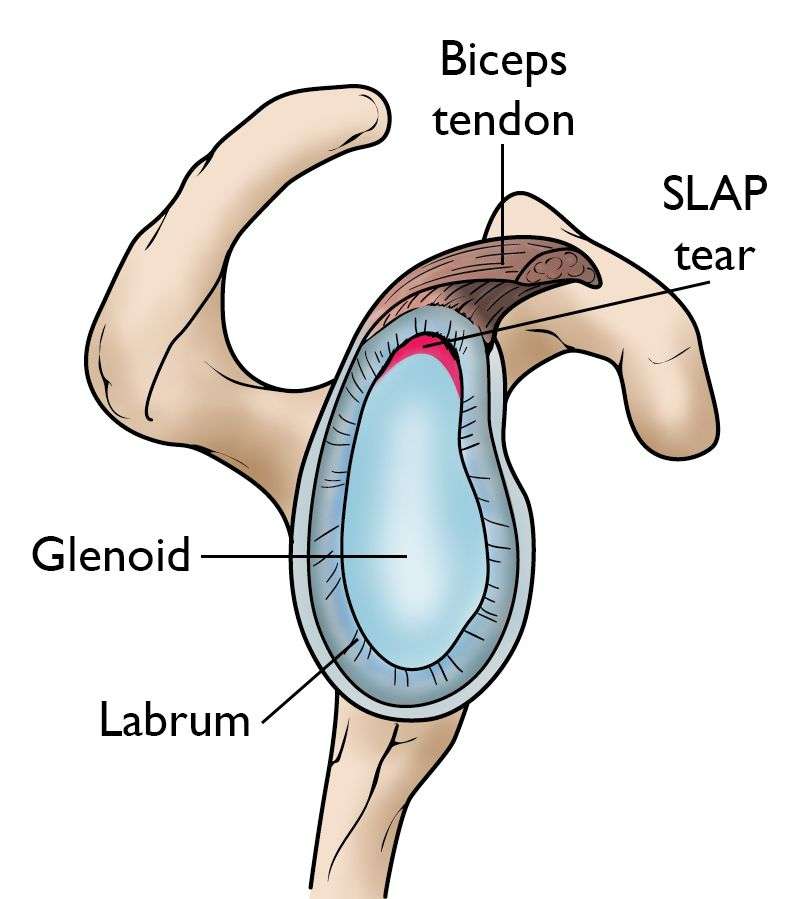
This cross-section view of the shoulder socket shows a typical SLAP tear.
Cause
Injuries to the superior labrum can be caused by acute trauma or by repetitive shoulder motion. An acute SLAP injury may result from:
- A motor vehicle accident
- A fall onto an outstretched arm
- Forceful pulling on the arm, such as when trying to catch a heavy object
- Rapid or forceful movement of the arm when it is above the level of the shoulder
- Shoulder dislocation
People who participate in repetitive overhead sports, such as throwing athletes or weightlifters, can experience labrum tears as a result of repeated shoulder motion.
Many SLAP tears, however, are the result of a wearing down of the labrum that occurs slowly over time. In patients over 30 to 40 years of age, tearing or fraying of the superior labrum can be seen as a normal process of aging. This differs from an acute injury in a younger person.
SLAP Classification
- I Labral and biceps fraying, anchor intact (11% of cases)
- II Labral fraying with detached biceps tendon anchor (41% of cases)
- III Bucket handle tear, intact biceps tendon anchor (33% of cases) (Biceps separates from bucket handle tear)
- IV Bucket handle tear with detached biceps tendon anchor (15% of cases) (Biceps remains attached to bucket handle tear)
- V Type II + anteroinferior labral extension (Bankart lesion)
- VI Type II + unstable flap
- VII Type II + MGHL injury
- VIII Type II + posterior extension
- IX Circumferential X Type II + posteroinferior extension (reverse Bankart)
Symptoms
The common symptoms of a SLAP tear are similar to many other shoulder problems. They include:
- A sensation of locking, popping, catching, or grinding
- Pain with movement of the shoulder or with holding the shoulder in specific positions
- Pain with lifting objects, especially overhead
- Decrease in shoulder strength
- A feeling that the shoulder is going to “pop out of joint”
- Decreased range of motion
- Pitchers may notice a decrease in their throw velocity, or the feeling of having a “dead arm” after pitching
Doctor Examination
Medical History
Your doctor will talk with you about your symptoms and when they first began. If you can remember a specific injury or activity that caused your shoulder pain, it can help your doctor diagnose your shoulder problem — although many patients may not remember a specific event. Any work activities or sports that aggravate your shoulder are also important to mention, as well as the location of the pain, and what treatment, if any, you have had.
Physical Examination
During the physical examination, your doctor will check the range of motion, strength, and stability of your shoulder.
He or she may perform specific tests by placing your arm in different positions to reproduce your symptoms. Your doctor may also examine your neck and head to make sure that your pain is not coming from a “pinched nerve.”
The results of these tests will help your doctor decide if additional testing or imaging of your shoulder is necessary.

Imaging Tests
X-rays. This imaging test provides clear pictures of dense structures, like bone. The labrum of the shoulder is made of soft tissue so it will not show up on an x-ray. However, your doctor may order x-rays to make sure there are no other problems in your shoulder, such as arthritis or fractures.
Magnetic resonance imaging (MRI) scans. This test can better show soft tissues like the labrum. To make a tear in the labrum show up more clearly on the MRI, a dye may be injected into your shoulder before the scan is taken.
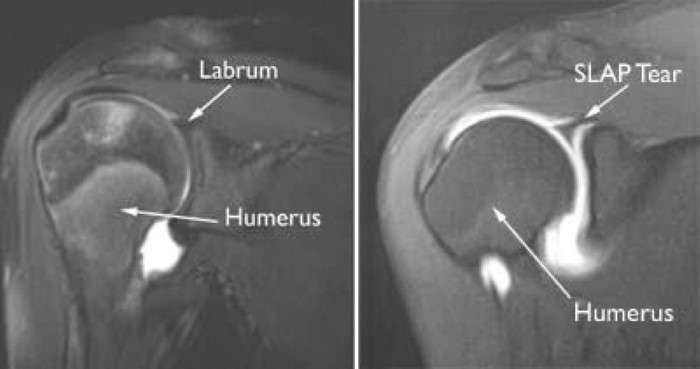
(Left) An MRI image of a healthy shoulder. (Right) This MRI image shows a tear in the labrum.
Treatment
Nonsurgical Treatment
In most cases, the initial treatment for a SLAP injury is nonsurgical.
Nonsteroidal anti-inflammatory medication. Drugs like ibuprofen and naproxen reduce pain and swelling.
Physical therapy. Specific exercises will restore movement and strengthen your shoulder. Flexibility and range-of-motion exercises will include stretching the shoulder capsule, which is the strong connective tissue that surrounds the joint. Exercises to strengthen the muscles that support your shoulder can relieve pain and prevent further injury. This exercise program can be continued anywhere from 3 to 6 months, and usually involves working with a qualified physical therapist.
Surgical Treatment
Your doctor may recommend surgery if your pain does not improve with nonsurgical methods.
Arthroscopy. The surgical technique most commonly used for treating a SLAP injury is arthroscopy. During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. The camera displays pictures on a video monitor, and your surgeon uses these images to guide miniature surgical instruments.
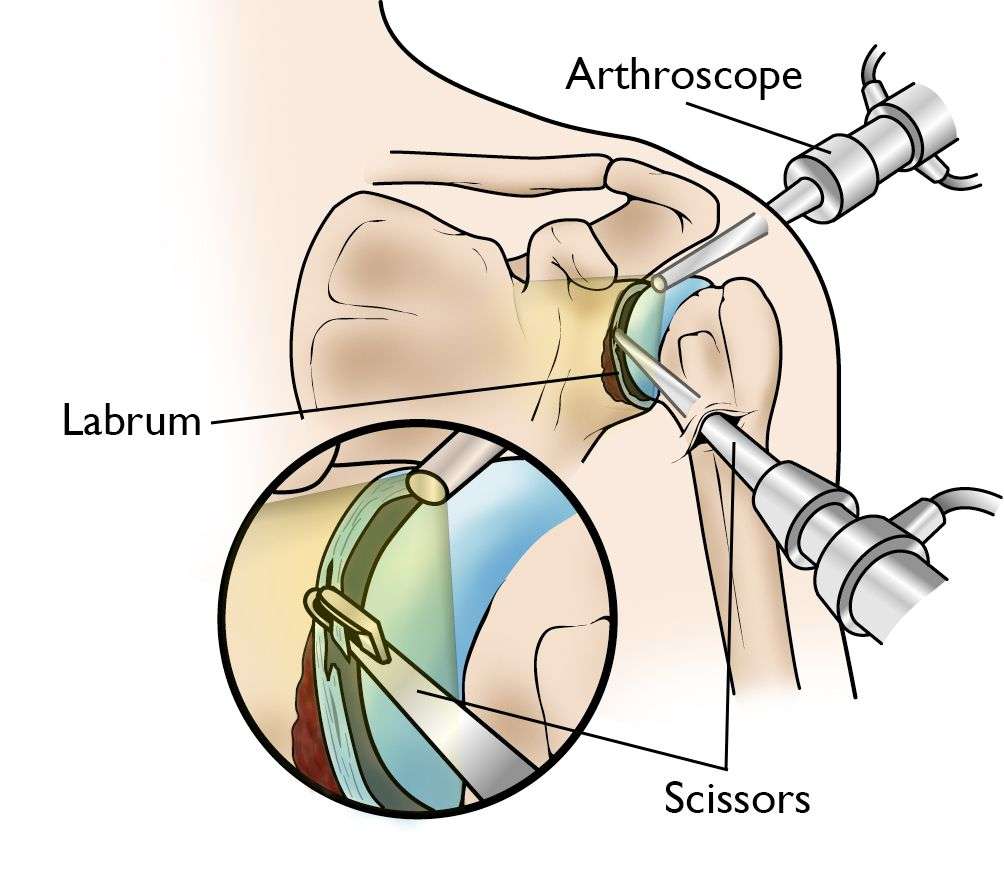
During arthroscopy, your surgeon inserts the arthroscope and small instruments into your shoulder joint.
Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions (cuts), rather than the larger incision needed for standard, open surgery.
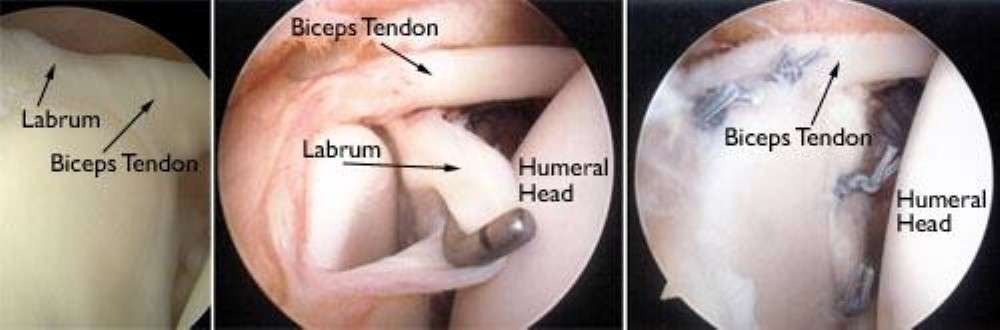
(Left) An arthroscopic view of a healthy labrum. (Center) In this image, the surgeon uses a small instrument to evaluate a large SLAP tear. (Right) The labrum has been reattached with sutures.
Treatment options. There are several different types of SLAP tears. Your surgeon will determine how best to treat your SLAP injury once he or she sees it fully during arthroscopic surgery. This may require simply removing the torn part of the labrum or reattaching the torn part using sutures. Some SLAP injuries do not require repair with sutures; instead, the biceps tendon attachment is released to relieve painful symptoms.
Your surgeon will decide the best treatment option based upon the type of tear you have, as well as your age, activity level, and the presence of any other injuries seen during the surgery.
Complications. Most patients do not experience complications from shoulder arthroscopy. As with any surgery, however, there are some risks. These are usually minor and treatable. Potential problems with arthroscopy include infection, excessive bleeding, blood clots, shoulder stiffness, and damage to blood vessels or nerves.
Your surgeon will discuss the possible complications with you before your operation.
Rehabilitation. At first, your shoulder needs to be protected while the repaired structures heal. To keep your arm from moving, you will most likely use a sling for 2 to 6 weeks after surgery. How long you require a sling depends upon the severity of your injury and the complexity of your surgery.

Wearing a sling will protect your shoulder after surgery.
Once the initial pain and swelling has settled down, your doctor will start you on a physical therapy program that is tailored specifically to you and your injury.
In general, a therapy program focuses first on flexibility. Gentle stretches will improve your range of motion and prevent stiffness in your shoulder. As healing progresses, exercises to strengthen the shoulder muscles and the rotator cuff will gradually be added to your program. This typically occurs 6 to 10 weeks after surgery.
Your doctor will discuss with you when it is safe to return to sports activity. In general, throwing athletes can return to early interval throwing 3 to 4 months after surgery.
Outcomes
The majority of patients report improved shoulder strength and less pain after surgery for a SLAP tear.
Because patients have varied health conditions, complete recovery time is different for everyone.
In cases of complicated injuries and repairs, full recovery may take several months. Although it can be a slow process, following your surgeon’s guidelines and rehabilitation plan is vital to a successful outcome.

