What is shoulder separation?
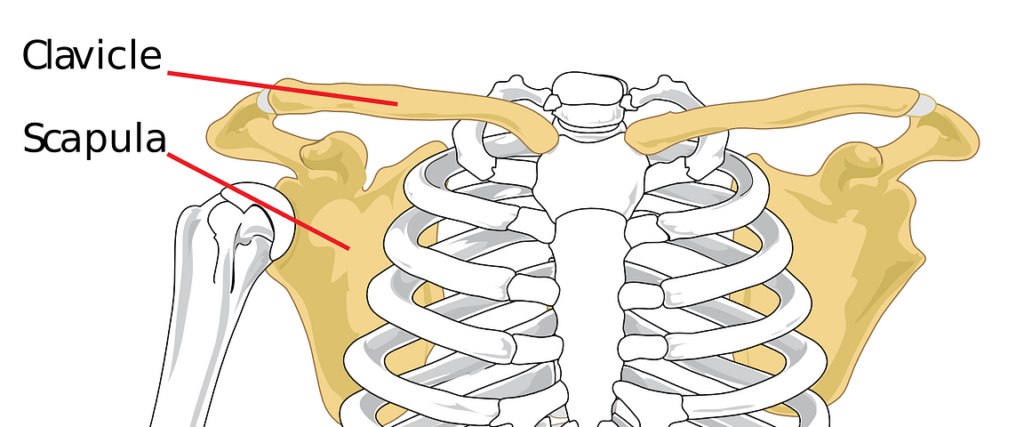
A shoulder separation is not truly an injury to the shoulder joint. The injury involves the acromioclavicular joint (also called the AC joint). The AC joint is where the collarbone (clavicle) meets the highest point of the shoulder blade (acromion). Acromioclavicular joint (ACJ) injuries are prevalent sporting injuries. Acute traumatic injuries occur with contact and collision sports, horse riding and motorsports.
What are the causes?
Repetitive traumatic injuries occur with overhead sports, boxing and weightlifting. Most of these injuries can be managed with rest and activity modification. The most common cause for separating the AC joint is from a fall directly onto the shoulder. The fall injures the ligaments that surround and stabilise the AC joint.
If the force is severe enough, this will tear the ligaments. This induces the separation of the collarbone from the shoulder blade. The arm with the shoulder blade moves downward from the weight of the arm. This creates a bump or bulge above the shoulder.
The injury can range from a mild sprain without a bump to complete dislocation. Good pain-free function often returns even with a huge bump. The greater the deformity, the longer it takes for the pain-free function to return.
There are six types but can be categorised into three categories:
• Category 1: A sprain that can be managed with physiotherapy and exercises. The collarbone is in place and looks normal on X-rays. (Grade I and II in the video below)
• Category 2: An injury tears the AC ligament and sprains or slightly tears the coracoclavicular (CC) ligament, putting the collarbone out of alignment to some extent with a smaller bump. This can be managed non-operatively or by surgery. Prof Imam or a team member will assess you and manage accordingly. (Grade III in the Video)
• Category 3: The most severe shoulder separation completely tears both the AC and CC ligaments and puts the AC joint noticeably out of position, with a more significant bump. This is usually managed with surgery (Grade IV-VI in figure)
The most famous classification is the Rockwood classification as below:
The ACJ is a subcutaneous joint without a large sleeve of muscle protection. It is more prone to injury because the sternoclavicular joint is very stable. Direct and indirect trauma can cause ACJ injuries.
Rockwood classification of ACJ injuries into six grades
I
AC joint sprain
II
Subluxated ACJ with intact CC ligaments
III
Dislocated ACJ with disrupted CC ligaments
IV
Superiorly and posteriorly dislocated ACJ
V
Dislocated ACJ with100–300% separation
VI
ACJ dislocated and Inferiorly displaced under the Coracoid
How to manage these injuries?
The injury is easy to identify when it causes deformity. When there is less deformity, the location of pain and x-rays help the doctor make the diagnosis. Sometimes having the patient hold a weight in the hand can increase the deformation, causing the injury more evident on x-rays.
CT scan is the best form of imaging to appreciate the static bony displacement. However, clinical assessment is probably just as reliable. MRI can be helpful to assess soft tissue damage in the acute scenario. A Stryker notch view is also beneficial if a coracoid fracture is suspected (average distance between the collarbone and the blade with complete disruption of the ACJ).
What are the treatment options?
NON-OPERATIVE TREATMENT
Non-operative treatment of acute injuries includes simple analgesia, topical ice therapy and rest in a sling for comfort. The use of a supportive broad arm sling is preferable to a collar and cuff because it supports the elbow and supports the weight of the shoulder. It is recommended that the sling be discarded once the symptoms settle, usually within one week.
Physiotherapy focuses on dynamic blade stabilisation and activity-specific rehabilitation. Contact sports and heavy lifting can be started as comfortable, usually about 6 to 12 weeks post-injury.
Non-operative staged progression rehabilitation
Phase
Protocol
I
Pain control, immediate protective range of motion, and isometric exercises
II
Strengthening exercises using isotonic contractions
III
Unrestricted functional participation with the goal of increasing strength, power, endurance, and neuromuscular
Control
IV
Return to activity with sport-specific functional drills.
Local discomfort may be felt with activity for up to six months. The literature reports that, at one year, there is a 17% chance of reduced bench press strength, although 80% of those patients do not find that a problem.
SURGICAL TREATMENT
Surgery can be considered if pain persists or the deformity is severe. A surgeon might recommend trimming back the end of the collarbone so that it does not rub against the shoulder blade bone (acromion).
Where there is significant deformity, reconstructing the ligaments that attach to the underside of the collarbone is helpful. This type of surgery works well even if it is done long after the problem started. These operations can be done arthroscopically or open, with a plate or without. Sometimes, if a plate is used to assist with the surgery, it is usually removed after healing of the shoulder separation.
The shoulder will require rehabilitation to restore and rebuild motion, strength, and flexibility, whether treated conservatively or with surgery. The purported advantage of surgical intervention, consistently borne out in the literature, is the increased probability of anatomic restoration. However, the current literature has not demonstrated a correlation between anatomical correction and pain, strength, or motion improvement.
The surgical intervention aims to achieve a painless, stable shoulder with adequate mobility, strength, and muscle control for the individual desired level of activity and participation. Over 100 different surgical techniques have been published to treat acute and chronic ACJ injuries. This is an indication of the lack of consensus in the literature as to the optimal treatment strategy. The described techniques include:
• Primary repair of the CC ligaments.
• Augmentation with autogenous tissue like coracoacromial (CA) ligament.
• Augmentation with absorbable and nonabsorbable suture as well as synthetic material.
• CC stabilisation with metallic screws.
Many techniques have been described as open, arthroscopic, and varying combined approaches. Each of the different methods has been used insolation or in combination with one or more others.
How do we manage these?
Acute injury (< 1week):
◦ Assess and diagnose.
◦ Sling for comfort only, analgesia and rehabilitation with early active mobilization as comfortable
◦ Surgery indicated if: Clearly in agony with clavicle button-holed through trapezius; Overhead athlete; Neurovascular injury; Open injury
• 3-week review:
◦ Settling and improving – continue symptomatic management and gradually return to sports and manual activities. Arrange review at 3 months.
◦ Not coping – offer early surgical reconstruction •
3-month review:
◦ Returned to sports and little symptoms – discharge
◦ Not coping – offer surgical stabilization
Our preferred method
Current trends are towards anatomical restoration of the CC and AC ligaments with some form of biological enhancement. The trend is towards strong constructs that allow for early mobilisation and less risk of displacement. This is usually achieved by passing the graft through the isometric points of the CC ligaments in the clavicle and either through a drill-hole in the coracoid or looped under the coracoid. This is combined with a repair or reconstruction of the AC ligaments and repair of the delto-trapezial fascia. These techniques seem to show the best results, with lower complications. With advancing technologies, these will continue to evolve and improve.
The ideal reconstructive technique should:
1. Restore the anatomical CC and AC ligament constructs
2. Be strong but flexible to allow some motion in all planes at the ACJ
3. Allow early rehabilitation.
4. Biological
5. Avoid donor site morbidity
6. Avoid the need for routine removal
Based on the above criteria, our preferred method involves using a strong, washed, synthetic polyethene-tetra phthalate ligament, known as the Ligament Advancement Reinforcement System (LARS Ligament, Corin). We use an anatomical construct through the clavicle, with a reefing repair of the ACJ capsule and delto-trapezial fascia. The LARS ligament exceeds the tensile strength of the native CC ligaments and has been shown to encourage fibroblast and collagen ingrowth. We also transfer one of the ligaments to achieve proprioception and augment the repair.
Return to Sports
Sports-specific rehabilitation starts within weeks of the rehabilitation process. The main aims are to apply the above rehabilitation principles in a sports-specific manner. For example, rugby players will use a rugby ball for proprioceptive work, and swimmers can do rehabilitation in water. Return to sport participation and competition is done in a graduated way, with input from the surgeon, therapist and strength and conditioning coaches. In our experience, this is usually achieved within 3-4 months for contact athletes and 6-9 months for overhead athletes] l. In our experience and practice reviews, horse riders and cyclists often return to sport less than three months post-surgery.


