Ganglion Cyst
What is a ganglion cyst?
A ganglion cyst is a benign but painful growth, usually on the hand or wrist. The pain often comes on at night or after constant use of the hand. Ganglion cysts can vary in size, growing up to three centimetres wide. While the position of the cyst doesn’t tend to change, the size may fluctuate over time, and some go away entirely without treatment.
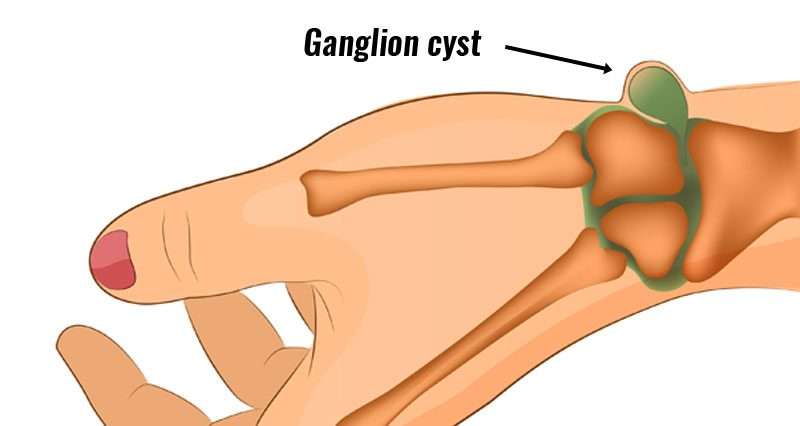
It usually occurs in the back of the wrist (dorsal) or volar (front). The fluid is clear and quite thick. They are thought to be related to changes in the lining of the joint, but not related to arthritis. Occasionally they communicate with the joint and/or a ligament in the joint.
Ganglion cysts are the most common mass or lump in the hand. They are not cancerous and, in most cases, are harmless. They occur in various locations, but most frequently develop on the back of the wrist.
These fluid-filled cysts can quickly appear, disappear, and change size. Many ganglion cysts do not require treatment. However, if the cyst is painful, interferes with function, or has an unacceptable appearance, there are several treatment options available.
Can a ganglion cyst be cured?
As previously mentioned, ganglion cysts sometimes go away on their own. If the cyst persists, treatment may be recommended to reduce the size or attempt to remove it completely. Unfortunately, if the cyst is removed, there is still a chance that it will come back, and you may need further treatment.
What are the symptoms?
A ganglion rises out of a joint, like a balloon on a stalk. It grows out of the tissues surrounding a joint, such as ligaments, tendon sheaths, and joint linings. Inside the balloon is a thick, slippery fluid, similar to the fluid that lubricates your joints.
Cysts usually form a visible nodule, although in some cases, if the cysts are small, they may not be noticeable. Many of them have no symptoms, but if they do press on a nerve, it can cause pain, tingling and muscle weakness.
How is a ganglion cyst diagnosed?
Usually, a ganglion cyst can be diagnosed by your GP with a physical examination. They may use a syringe to draw out fluid from the cyst. In some cases, they might refer you for an ultrasound or MRI to look at the inside of the lump and rule out other potential causes.
What causes a ganglion cyst?
The cause of ganglion cysts is unknown. They have been found to be more common in young people between the ages of 15 and 40 and to develop more in women. It is also more likely to be developed by people who use and overload the wrist. People who have arthritis may develop them more easily.
It is not known what triggers the formation of a ganglion. They are most common in younger people between the ages of 15 and 40 years, and women are more likely to be affected than men. These cysts are also common among gymnasts, who repeatedly apply stress to the wrist.
Ganglion cysts that develop at the end joint of a finger — also known as mucous cysts — are typically associated with arthritis in the finger joint, and are more common in women between the ages of 40 and 70 years.
Can ganglion cysts be prevented?
At the moment, it is not clear how to prevent ganglion cysts. The best thing to do is to see Prof Imam early on if you notice anything unusual.
How are ganglion cysts treated?
Initial treatment of a ganglion cyst is not surgical.
Observation. Because the ganglion is not cancerous and may disappear in time, if you do not have symptoms, your doctor may recommend just waiting and watching to make sure that no unusual changes occur.
Immobilization. Activity often causes the ganglion to increase in size and also increases pressure on nerves, causing pain. A wrist brace or splint may relieve symptoms and cause the ganglion to decrease in size. As pain decreases, your doctor may prescribe exercises to strengthen the wrist and improve range of motion.
Aspiration. If the ganglion causes a great deal of pain or severely limits activities, the fluid may be drained from it. This procedure is called an aspiration.
The area around the ganglion cyst is numbed and the cyst is punctured with a needle so that the fluid can be withdrawn.
Aspiration frequently fails to eliminate the ganglion because the “root” or connection to the joint or tendon sheath is not removed. A ganglion can be like a weed which will grow back if the root is not removed. In many cases, the ganglion cyst returns after an aspiration procedure.
Aspiration procedures are most frequently recommended for ganglions located on the top of the wrist. The risk of recurrence is 50%.
For many people, treatment will not be necessary, especially if there is no associated pain. The main job of the GP will be to reassure you that the lump is not caused by anything more serious. However, if the cyst is causing you pain, the GP may recommend treatment.
Surgical Treatment
Your doctor may recommend surgery if your symptoms are not relieved by nonsurgical methods, or if the ganglion returns after aspiration. The procedure to remove a ganglion cyst is called an excision.
Surgery involves removing the cyst as well as part of the involved joint capsule or tendon sheath, which is considered the root of the ganglion. Even after excision, there is a small chance the ganglion will return.
Excision is typically an outpatient procedure and patients are able to go home after a period of observation in the recovery area. There may be some tenderness, discomfort, and swelling after surgery. Normal activities usually may be resumed 2 to 6 weeks after surgery.
Special forms of Ganglions
Pearl Ganglion
Also known as A1 pulley ganglion or Pearl ganglion
Why does it occur?
It is a fluid-filled sac that happens at the base of a finger on its front surface. They are thought to be related to changes in the lining of the joints and tendon sheaths.
Symptoms
A painless lump that comes and goes in size. The outline is quite smooth and may feel tense, like a small ball or balloon (cystic).
Clinical Examination
A seed ganglion has quite typical features both in its location and appearance. With the lights turned down and a pen torch is shone through the lump, it transilluminates.
Investigations
Usually none. In unusual situations, an ultrasound scan will be helpful.
Non-operative treatment
Ganglions can be aspirated under local anaesthetic. A needle is then introduced into the lump, and the fluid is sucked away. However, they can be quite small and difficult to aspirate with a needle.
Operative treatment
If the lump has reappeared six weeks after aspiration or was too small to aspirate, we usually recommend surgery. The surgery is a day case procedure usually under local anaesthetic and takes about 10 minutes. A tourniquet is used, which is like a blood pressure cuff around the upper arm that prevents blood from obscuring the surgeons’ view. It is quite tight but well tolerated for up to 20 minutes.
Local anaesthetic is infiltrated under the skin in line with the incision over the lump. Once numb, the skin is incised, and then the underlying fat is retracted. Care is taken not to injure nerves and blood vessels. At the base of the wound is the ganglion wall. The ganglion is dissected, taking care not to puncture it. The base of the ganglion is identified and excised. The skin is sutured, and a bulky dressing is applied.]
Post-operative rehabilitation
The patient is fit to go home soon after the operation. The anaesthetic will wear off after approximately 6 hours. Simple analgesia usually controls the pain and should be started before the anaesthetic has worn off. The hand should be elevated as much as possible for the first five days to prevent the hand and fingers swelling. Gently bend and straighten the fingers from day one. My preference is to remove the dressing for two days. The wound is cleaned and redressed with a simple dressing. The sutures are removed at about ten days.
Return to activities of daily living
It is my advice to keep the wound dry until the stitches are out at ten days.
Return to driving:
The hand needs to have full control of the steering wheel and left hand the gear stick. It is probably advisable to delay returning to driving for at least seven days or even when the stitches are removed.
Return to work:
Everyone has different work environments.
Returning to heavy manual labour should be prevented for approximately 4 to 6 weeks. Early return to heavy work may cause the tendons and nerve to scar into the released ligament. Please ask your surgeon for advice on this.
Complications
Overall, greater than 90% are happy with the result. However, complications can occur.
Specific complications:
Recurrence: This is reported between 10 and 40%. We are not sure whether it is the same ganglion recurring or simply another one forming nearby.