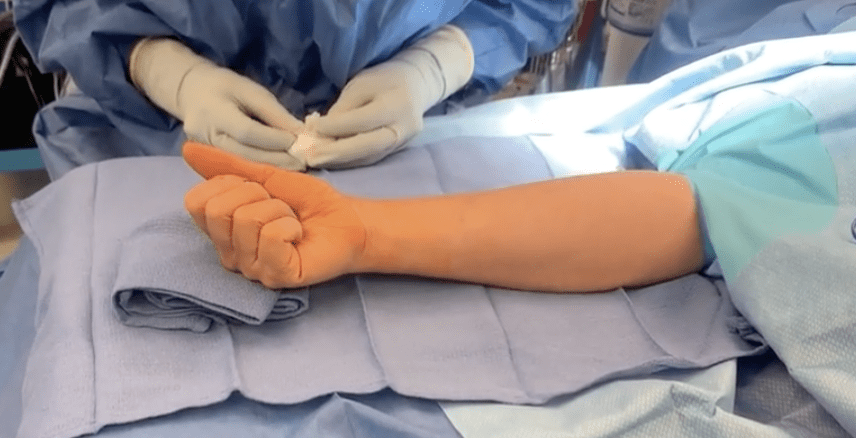
Complications following surgery
Here is a list of complications that may occur in arm surgery.
Most of the cases do not have complications, but you need to be aware that they might occur. I would be discussing these with you in person should you require surgery at the time of our consultation. I am also more than happy to see you for a separate consent clinic if you require more information than what we discussed and listed below.
This list does not aim to scare you or put you off surgery as most of our patients are very pleased with the results but do help explain what can go wrong.
A discussion is always required and is useful as it makes us all appreciate that things can go wrong. I tend to apply the family and friends test whenever I am discussing the best option for you.
Clinical governance means providing the best care possible to the patient sitting in front of me and simply means will I be doing the same procedure or intervention to a friend or family member? If yes, then I would discuss that option with you.
Surgery should always be the last resort, having explored non-operative options including:
Do nothing, and the natural history of the condition unfolds
Rest and Splinting
Physiotherapy or hand therapy
Injections – cortisone, Platelets, stem cells, hyaluronic acid etc.
Here are some of the commonly discussed complications, but fortunately, in the arm, they are all quite rare.
Failure to resolve symptoms
We aim to improve your symptoms. On rare occasions, unfortunately, this may not occur and may be related to your case complexity.
Infection
The arm has an excellent blood supply, and therefore, post-operative infections are rare. Signs of infection would be redness, pain and swelling around the surgical site and developing after a few days (3-10 days) rather than immediately post-operation (1-2 days), which may be a normal reaction to surgery. Very occasionally, about 1 in 20 patients develop a small pinhead size of puss around the white dissolvable suture. This usually needs popping. It seems to be a poorly understood reaction to the dissolving stitch rather than an infection. If this occurs, simply send me a photo for reassurance.
If you have any concerns, please do not hesitate to contact me to review your wounds.
Most infections are superficial and can be easily treated with dressings or oral antibiotics. More severe cases may have a deep infection that requires a further operation to clean the wound or intravenous antibiotics as an inpatient.
These can be a problem in cases of replacement surgery. That is why it important to read our before surgery section
Ongoing pain
After any operation, there will be some pain. I would hope that the majority of discomfort will settle within the first few days of the operation. Depending upon the operation will depend upon the duration of post-operative pain. I will discuss this with you in the clinic if needed.
Swelling
All wounds swell after an operation, and the majority of swelling will have settled within the first week. Swelling after 2-4 weeks would need reviewing.
Bleeding
General ooze into the dressings may occur after an operation and is preferable to allowing the blood to remain in the wound, developing a haematoma (collection of blood) that can be prone to infection. Continuing bleeding after a few days would be very rare and would need review. A haematoma is a collection of blood under the skin and, if very large, rare in the upper limb would need releasing.
Scarring
Scar’s on the arms heal very well and are often barely noticeable. I tend to use a dissolvable stitch that dissolves after 2-4 weeks. On the palm, the stitches are usually interrupted and exposed stitches, whereas, on the back of the hand, they are under the skin and called subcuticular and cannot be seen, apart from two small knots at either end of the wound. My carpal tunnel stitch, however, tends to be subcuticular.
Bruising
Bleeding is inevitable after an operation, and sometimes this comes to the skin like a bruise. After a few days, a red bruise will turn black and blue before fading after a week or two.
Weakness
Weakness can be due to ongoing pain or a restriction of movement. Hopefully, most operations would maintain or increase strength, but occasionally patients can experience a mild degree of weakness. Severe weakness would be very rare.
Stiffness
After an operation, you may develop internal scarring, which in turn can restrict the range of movement of a joint. We would hope that most of the movement would return, but there may sometimes be a permanent restriction of movement. This does not usually cause much in the way of the functional problem.
Nerve injury
Nerves are small soft electrical “wires” that transport information to and from the brain from the periphery. Most nerves are mixed and have a motor (movement) and sensory (sensation) roles.
The motor component sends information to a muscle to tell it to contract. In contrast, the sensory component carries information from the skin about various sensations, including touch and pain.
Nerves may be injured as part of an injury but can be injured during surgery on very rare occasions. We take particular care to identify all important nerves during your surgery and retract them out of harm’s way. Despite this very rarely, they can still be injured.
If a nerve is injured, then the function may be affected. Some nerves are bruised (neuropraxia), and recovery may occur over a few months. Some nerves are permanently injured, and therefore, recovery is not possible, leaving areas of numbness and weakness to a muscle or group of muscles.
Neuroma
A neuroma occurs when a nerve is injured. The end of the nerve that is cut or damaged overgrows and forms a knot of nerve tissue that is very painful. Neuromas can be difficult to treat. Common treatments include therapy to desensitise the area, neuromodulation (using various techniques including vibration to re-educate and settle the nerve end) and ultimately surgery to locate the neuroma and bury it into a protective environment such as an adjacent bone or muscle.
Numbness
Numbness may occur if a sensory nerve is bruised after an operation and recovers over a 3-6-month period. If a nerve is cut, then the sensation may never recover.
Tendon injury
Tendons are cord-like structures that connect muscles to bone, allowing the muscle contraction to pull on the tendon and move the bone and joint. Tendons can be injured in surgery, and this would affect the joint(s) moving. Tendons are identified during the operation and protected, but very rarely, they can be injured. Some tendons can rupture spontaneously, and this can occur after a wrist fracture treated in a POP, or if a tendon passes over a rough, sharp edge of a bone or in some diseases such as rheumatoid arthritis.
Complex Regional Pain Syndrome (CRPS)
Complex Regional Pain Syndrome (CRPS) can occur after any injury, including surgery. As its name suggests, it is a complex condition with many factors at play. To reduce the risk of it occurring, we always recommend moving all joints as soon as possible after surgery and keeping them moving. Sometimes fingers and wrists are immobilised after an injury or operation and cannot be moved, but all the other joints should be kept moving.
CRPS causes redness, swelling and pain. In severe cases, the hand may become red and shiny, and abnormal hair growth forms. In our practice, this is very rare and much less than 0.5% – based on the last three years’ cases. We often use hand therapists post-operatively, and I am sure they are the reason for my low rates of CRPS.
Instability
Ligaments connect joints; ligaments can be injured in an accident or during surgery. I am aware where the important ligaments are in the hand and will avoid injuring them. However, sometimes after joint replacements or joint reconstructions, the ligaments do not function as well, causing instability (abnormal excessive movement of a joint) and ultimately dislocation when the joint comes out of the socket.
Dislocation
This occurs when a joint – artificial or the original joint comes out of place. Pain and reduced movement occur. The treatment is usually to put the joint back into place and stabilise with either a splint or, on rare occasions, another operation to revise the artificial joint or stabilise it.
Joint replacement
Joints that are replaced are artificial and may wear out over time. In such cases, they may need revising to a new implant.
Furthermore, when placing an implant into the body, the surrounding bones can be fractured, and so great care is taken to avoid this. Depending upon which bone is affected would depend upon what is required to resolve the situation.
Compartment Syndrome
After an injury or major operation, swelling can occur in the limb. The swelling may be conscripted by the surrounding firm fibrous bags inside the hand and arms.
Pain starts to develop along with swelling, and each hour gets worse and worse and is disproportional to the pain one would normally expect. Tingling in the fingers is a very late stage, and extreme pain is the main symptom, particularly on moving the fingers. This is a surgical emergency, and the pressure needs relieving by a trained doctor, often removing the dressings and cast but sometimes releasing the tight fibrous bags in the arm with open surgery.
Cold intolerance
Cold intolerance is poorly understood and can occur as a result of injury to the fingers, including surgery. An abnormal response may occur to cold environments and cause a colour change, pain, stiffness and altered sensation. It generally improves after injury, but symptoms after 18 months may be permanent.
Non-union / Mal union
Bones usually heal without problems. Bones need to heal in various situations, including after a fracture, after an operation to fuse a joint or after an osteotomy (intentional operation to cut a bone to improve its shape). However, some bones are prone to not healing either due to an injury or after an operation. If a bone fails to heal, it is called a non-union, and if it heals in an abnormal position, it is called a malunion. Non-unions can be either painful or painless.
After a joint fusion operation, the bone does not heal and is painful; it may need further surgery. If a non-union is painless, it may be stable and not require intervention. Smoking affects bone healing and should be stopped several months before surgery if the outcome is to be optimised.
For specific complications, please check the consents section in downloads.