Skier’s thumb
Ulnar Collateral Ligament Tears of the Thumb
Ulnar Collateral Ligament Tears of the Thumb
Patients with UCL tears present with pain, stiffness, tenderness, and swelling of the MCP joint.
The defining symptom, however, may be marked pinch weakness.
On examination, there is discrete tenderness over the ulnar joint line, at the ulnar side of the metacarpal neck, and most classically at the volar ulnar base of the proximal phalanx.
• Physical examination is critical in establishing the need for surgical treatment by distinguishing between a partial and a complete ligament tear.
• A valgus stress examination comparing the stability of the injured versus the uninjured UCL is the best method to detect a complete tear. The stress test may be aided by live fluoroscopy and the use of a local anesthetic block.
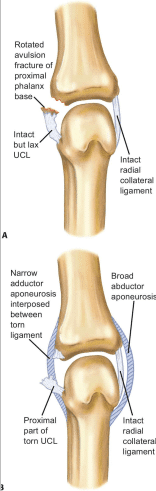
The presence of an associated fracture should not deter the examiner from performing a stress test. Nondisplaced avulsion fractures at the insertion site of the proper collateral ligament may coexist with a complete ligament tear.
The results of the stress test are based on angular instability of the joint and the quality of the “end point.”
Laxity of more than 30 degrees in extension and 15 degrees in flexion as compared to the contralateral side should be highly suggestive of a complete tear of the UCL.
The presence of fullness or a palpable mass on the ulnar aspect of the metacarpal head and neck, representing a stener lesion, is strongly suggestive of a completely disrupted and retracted UCL.
Volar subluxation of the MCP joint signifies loss of the dorsal volar stabilizing effect of the collateral ligament and is also consistent with a complete tear.
Surgical Treatment
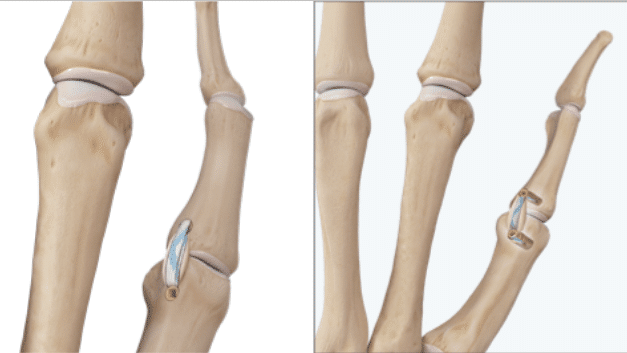
Thumb UCL Repair with InternalBrace Ligament Augmentation
• Injuries associated with a Stener lesion warrant open repair.
• Partial tears of RCL are best managed by cast immobilization, whereas complete tears associated with palmar subluxation require open surgical repair of the ligament and dorsal capsule.
• Arthroscopy can also be a useful adjunct to open procedures, as it allows a more thorough débridement and evaluation of concomitant pathology.
• A regional anesthetic combined with light intravenous sedation is generally adequate for the procedures detailed in the following text.
Thumb UCL Repair with InternalBrace Ligament Augmentation
Contraindications to this technique are painful arthritis of the thumb metacarpophalangeal joint, cysts or hardware within the metacarpal or proximal phalanx that would prevent satisfactory anchor placement, open physes and infection.
POSTOPERATIVE MANAGEMENT
True ligament-to-bone healing is necessary, so 6 weeks of postoperative thumb spica/ Orthotic immobilization is critical to success. All unrestricted activities are permitted at 8 weeks.
Self-care and follow-up
• Dressing and Wound Care
After surgery, you will be in a bulky dressing (bandage) with a plaster splint that covers your thumb, wrist and forearm. The splint is similar to a cast. The splint cannot be removed and must be kept dry.
When showering or bathing, cover the splint and your hand with a plastic bag to keep everything dry. The splint protects the incision and the surgical reconstruction, as well as lessen swelling.
Elevate your hand above your heart as much as possible to lessen swelling and pain. Pillows and blankets under the arm are helpful when you go to sleep. Mild to moderate after surgery is common.
The splint must remain in place until your follow-up appointment 10- 14 days after surgery.

You will likely have one 2-3 cm surgical incision on the inside of your thumb near your webspace.
• Driving
Do not drive if you are taking narcotic pain medication. It is not safe. The medicine can make you sleepy and delay your reaction
Once you are no longer taking the medicine, you may drive as soon as you can comfortably grip the steering wheel with both hands. It is generally best to avoid long drives until the initial dressing and plaster splint is removed.
• Activity
Right after surgery, you may begin gentle finger exercises.
However, you will be unable to move the base of your thumb or your wrist because of the splint. You can use your hand for very light activities of daily living, such as eating, writing, typing, getting dressed, and brushing your teeth.
Gripping, grasping, or pinching with the thumb are prohibited until your surgeon or therapist says you may do these things. Premature return to these activities may cause failure of the repair.
• Follow-Up Plan
You will have a follow-up appointment with the surgical team scheduled 10-14 days after surgery.
At that visit:
You will be placed into custom removable brace by our hand therapist to protect your repair as it heals.
You will wear the brace full-time (including night-time) to protect your repair for 4 more weeks.
The brace may be removed for showering and gentle active motion exercises directed by the therapist.
At 6 weeks after surgery, the supportive brace should be worn with activities, but you may do light tasks, such as typing without it. You are still advised to avoid gripping, grasping and twisting with your thumb.
Three months after surgery, you will not need to use any braces or splints to support your hand and fingers. At this time, you may grip, grasp, and twist using your thumb. You may also begin strengthening exercises if needed.
Most patients have minimal pain by 6 weeks after surgery, with nearly full thumb and hand motion by 3 months.
Your symptoms will continue to improve by working in therapy. It is important that you consistently work with your therapist to optimize motion and strength after surgery.
Patients usually regain full motion and strength in their operative thumb.


