Trigger Finger / Thumb
What is it?
Trigger finger is a condition that causes pain, stiffness, and a sensation of locking or catching when you bend and straighten your finger. The condition is also known as “stenosing tenosynovitis.” The ring finger and thumb are most often affected by trigger finger, but it can occur in the other fingers, as well. When the thumb is involved, the condition is called “trigger thumb.”
A trigger finger is a condition that affects the tendons that bend the fingers. When the tendon sheath is inflamed, it makes finger extension or flexion difficult. This can cause the fingers to lock or trigger suddenly. The medical term for it is tenosynovitis.
Why does it occur?
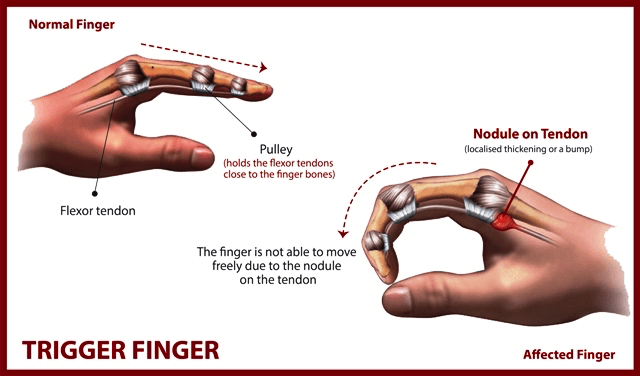
The tendons in the fingers that cause the fingers to bend (flex) may develop a nodule.
Finger flexor tendons travel in a slippy sheath along with the finger, and the tendon slides in and out as the finger bends and straightens. The sheath lubricates the tendon and also prevents bowstringing of the tendons as the finger bends. In cases of trigger finger, a nodule develops on the tendon. As the finger bends, the nodule passes out of the sheath into the palm. As the finger straightens, the nodule attempts to pass back into the sheath but becomes locked at its mouth. It is preventing the finger from fully straightening. The finger may be forcibly straightened with a click but should be avoided.
While the causes of trigger finger are not well known, several factors may increase your risk for developing the condition.
These include:
⦁ Medical conditions. Trigger finger is more common in people with certain medical conditions, such as diabetes and rheumatoid arthritis.
⦁ Forceful hand activities. The condition is known to occur after forceful use of the fingers and thumb.
Prognosis
It is not common for trigger fingers to spontaneously resolve. If it is not treated, it is likely to be a painful discomfort. If the finger gets trapped, it could cause permanent stiffness.
What are the symptoms?
Symptoms of trigger finger often start without a single injury. They may follow a period of heavy or extensive hand use, particularly pinching and grasping activities.
Symptoms may include:
⦁ A tender lump at the base of the finger on the palm side of the hand
⦁ A catching, popping, or locking sensation with finger movement
⦁ Pain when you bend or straighten the finger
Stiffness and locking tend to be worse after periods of inactivity, such as when you wake up in the morning.
In a severe case, the involved finger may become locked in a bent position.
Medical tests
The diagnosis can normally be made based on the patients’ medical history and symptoms. A physical exam is normally carried out to assess the stiffness and sensitivity of the affected fingers. The doctor may choose to do an ultrasound to check the swelling or they may carry out specific tests if they think it may be related to a different condition.
What causes it?
There is no clear cause for this condition, but it is thought to be related to rheumatoid arthritis, gout, or diabetes. It is more common in women and people aged between 40 and 60 years old. People who regularly carry out activities that require repetitive phalange flexion and extension for long periods of time, or put intense external pressure on a finger, are more likely to be affected by trigger finger.
How can it be prevented?
Tenosynovitis can only partially be prevented. If it is due to an underlying condition (rheumatoid arthritis for example) that causes thickening of the finger tendon sheaths and causes involuntary movements and pain, it should be treated before it causes trigger finger. It may also be caused by a tendon mechanical overload. Certain movements should be avoided, and exercises should be carried out to strengthen the tendons.
Recommendations include:
⦁ Limit repetitive or forced finger activities
⦁ Alternate activities
⦁ Rest between tasks
⦁ Try to not force movement
⦁ Regularly exercise fingers and palm.
What is the treatment?
Trigger finger treatment normally involves alleviating tendon pressure and enabling finger movement without any discomfort. A splint or anti-inflammatory medications are often used. If these treatments don’t work, surgery may be resorted to.
Non-operative treatment
Babies that are affected have a 90% chance of the condition settling by 12 months old. If it fails to settle after this and is troublesome, then surgery is indicated. Also, if the thumb is locked in a child, then this should be operated on early to prevent joint problems.
In adults, a steroid injection into the sheath may lubricate and also damp down the inflammation. Steroid injections can be repeated once. Further attempts may damage the tendon, and surgery would be advised after one or two failed injections.
So Options are:
Initial treatment for a trigger finger is usually nonsurgical.
Rest. Resting your hand and avoiding activities that make it worse may be enough to resolve the problem.
Splinting. Wearing a splint at night to keep the affected finger or thumb in a straight position while you sleep may be helpful.
Exercises. Gentle stretching exercises can help decrease stiffness and improve range of motion in the involved digit.
Medications. Over-the-counter medications, such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs), can help relieve pain and inflammation.
Steroid injections. Corticosteroid, or cortisone, is an anti-inflammatory agent that can be injected into the tendon sheath at the base of the trigger finger. A steroid injection may resolve the triggering over a period of one day to several weeks. If symptoms do not improve with time, a second injection may be given. If two injections do not help the problem, surgery may be considered.
Steroid injections are less likely to be effective in patients with diabetes, but may still help avoid surgery. They can cause a short-term rise in blood sugar, so glucose levels in diabetic patients should be monitored after injection.
Operative treatment
The surgery is a day case procedure usually under local anaesthetic and takes about 10 minutes. A tourniquet is not often needed.
Local anaesthetic is infiltrated under the skin in line with the incision at the base of the digit on its flexor (front) surface. Once numb, the skin is incised, and then the underlying fat is retracted. Care is taken not to injure nerves and blood vessels to the digit. At the base of the wound is the flexor sheath.
The mouth of this structure (A1 pulley) needs to be released to allow the tendon and its nodule to glide in and out without catching. The nodule is not removed. The skin is sutured with absorbable sutures, and a bulky dressing is applied.
Post-operative rehabilitation
The patient is fit to go home soon after the operation. The anaesthetic will wear off after approximately 6 hours. Simple analgesia usually controls the pain and should be started before the anaesthetic has worn off.
The hand should be elevated as much as possible for the first five days to prevent the hand and fingers swelling. Gently bend and straighten the fingers from day 1. My preference is to remove the dressing at two days. The wound is cleaned and redressed with a simple dressing. Avoid forced gripping or lifting heavy objects for 2-3 weeks. The sutures dissolve at about two weeks. You should notice an improvement in symptoms within a few days, but the final result may be realised at about three months.
Return to activities of daily living
It is my advice to keep the wound dry until the wound heals at about 7-10days.
Return to driving:
The hand needs to have full control of the steering wheel and left hand the gear stick. It is probably advisable to delay returning to driving for a few days.
Return to work:
Everyone has different work environments.
Returning to heavy manual labour should be prevented for approximately 4 to 6 weeks. Early return to heavy work may cause the tendons and nerve to scar into the released ligament. Please ask your surgeon for advice on this.
Complications
Overall, greater than 95% are happy with the result. However, complications can occur.
Specific complications:
Failure to completely resolve the symptoms (approximately 1% – this may be due to failure to completely release the area that is catching). This should be rare but may be released again.
Injury to the blood vessels and nerves to the finger (less than 1%). This may leave one side of the finger numb. If this occurs, the wound should be explored, and if injured, the nerve repaired.