Shoulder Instability
What is shoulder instability?
Shoulder instability is a common shoulder problem, and regularly seen by therapists, surgeons, sports doctors and emergency clinicians. Its management can be complex and multidisciplinary.
A dislocated shoulder
The shoulder joint is the body’s most mobile joint. It can turn in many directions, but this advantage also makes the shoulder an easy joint to dislocate.
A partial dislocation (subluxation) means the head of the upper arm bone (humerus) is partially out of the socket (glenoid). A complete dislocation means it is all the way out of the socket. Both partial and complete dislocations cause pain and unsteadiness in the shoulder.
Symptoms
Common symptoms of chronic shoulder instability include:
- Repeated shoulder dislocations
- Repeated instances of the shoulder giving out
- A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just hanging there
- Pain caused by shoulder injury
Treatment
Prof Imam will place the ball of the upper arm bone (humerus) back into the joint socket. This process is called a closed reduction. Severe pain stops almost immediately once the shoulder joint is back in place
Rehabilitation
Prof Imam may immobilize the shoulder in a sling or other device for several weeks following treatment. Plenty of early rest is needed. The sore area can be iced 3 to 4 times a day.
After the pain and swelling go down, your doctor will prescribe rehabilitation exercises for you. This help restore the shoulder’s range of motion and strengthen the muscles. Rehabilitation may also help prevent dislocation of the shoulder again in the future.
Rehabilitation will begin with gentle muscle toning exercises. Later, weight training can be added.
If shoulder dislocation becomes a recurrent problem, a brace can sometimes help. However, if therapy and bracing fail, surgery may be needed to repair or tighten the torn or stretched ligaments that help hold the joint in place, particularly in young athletes.
At times, the recurrently dislocating shoulder can result in some bone damage to the humerus or shoulder socket. If your surgeon identifies some bone damage, he or she may recommend a bone transfer type of surgery.
Chronic Shoulder Instability
The shoulder is the most moveable joint in your body. It helps you to lift your arm, to rotate it, and to reach up over your head. It is able to turn in many directions. This greater range of motion, however, can cause instability. Shoulder instability occurs when the head of the upper arm bone is forced out of the shoulder socket. This can happen as a result of a sudden injury or from overuse.
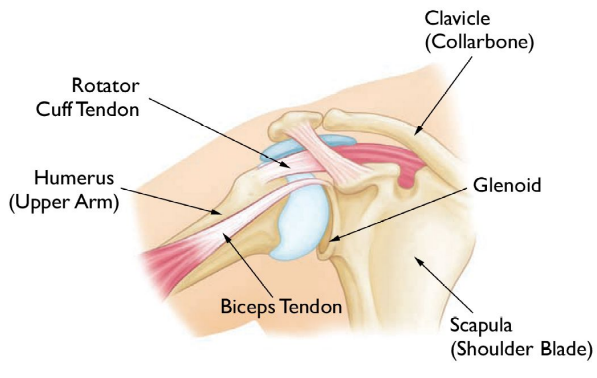
Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, it is called chronic shoulder instability. The head, or ball, of your upper arm bone, fits into a shallow socket in your shoulder blade. This socket is called the glenoid. Strong connective tissue, called the shoulder capsule, is the ligament system of the shoulder and keeps the head of the upper arm bone centred in the glenoid socket. This tissue covers the shoulder joint and attaches the upper end of the arm bone to the shoulder blade. Your shoulder also relies on strong tendons and muscles to keep your shoulder stable.
Description
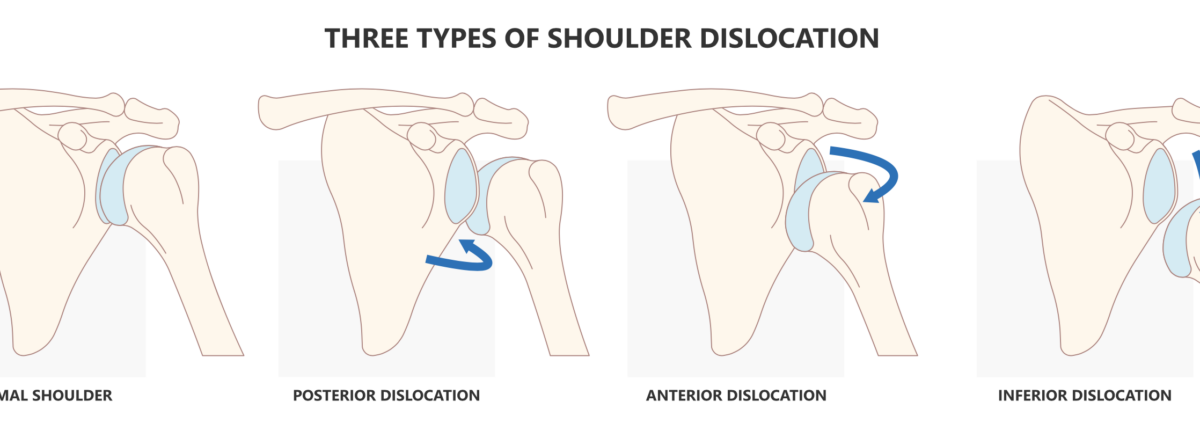
Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket.
Once the ligaments, tendons, and muscles around the shoulder become loose or torn, dislocations can occur repeatedly. Chronic shoulder instability is the persistent inability of these tissues to keep the arm centred in the shoulder socket.
Cause
There are three common ways that a shoulder can become unstable:
Shoulder Dislocation
Severe injury, or trauma, is often the cause of an initial shoulder dislocation. When the head of the humerus dislocates, the socket bone (glenoid) and the ligaments in the front of the shoulder are often injured. The labrum — the cartilage rim around the edge of the glenoid — may also tear. This is commonly called a Bankart lesion. A severe first dislocation can lead to continued dislocations, giving out, or a feeling of instability.
Repetitive Strain
Some people with shoulder instability have never had a dislocation. Most of these patients have looser ligaments in their shoulders. This increased looseness is sometimes just their normal anatomy. Sometimes, it is the result of repetitive overhead motion.
Swimming, tennis, and volleyball are among the sports requiring repetitive overhead motion that can stretch out the shoulder ligaments. Many jobs also require repetitive overhead work.
Looser ligaments can make it hard to maintain shoulder stability. Repetitive or stressful activities can challenge a weakened shoulder. This can result in a painful, unstable shoulder.
Multidirectional Instability
In a small minority of patients, the shoulder can become unstable without a history of injury or repetitive strain. In such patients, the shoulder may feel loose or dislocate in multiple directions, meaning the ball may dislocate out the front, out the back, or out the bottom of the shoulder. This is called multidirectional instability. These patients have naturally loose ligaments throughout the body and maybe “double-jointed.”
Symptoms
Common symptoms of chronic shoulder instability include:
• Pain caused by a shoulder injury
• Repeated shoulder dislocations
• Repeated instances of the shoulder giving out
• A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just “hanging there”
Imaging Tests
Your doctor may order imaging tests to help confirm your diagnosis and identify any other problems.
X-rays. These pictures will show any injuries to the bones that make up your shoulder joint.
Magnetic resonance imaging (MRI). This provides detailed images of soft tissues. It may help your doctor identify injuries to the ligaments and tendons surrounding your shoulder joint. Although nowadays the best option is an MR scan with a dye.
Treatment
Chronic shoulder instability is often first treated with nonsurgical options. If these options do not relieve the pain and instability, surgery may be needed.
Nonsurgical Treatment
Prof Imam will develop a treatment plan to relieve your symptoms. It often takes several months of nonsurgical treatment before you can tell how well it is working.
Nonsurgical treatment typically includes:
Activity modification. You must make some changes in your lifestyle and avoid activities that aggravate your symptoms.
Non-steroidal anti-inflammatory medication. Drugs like aspirin and ibuprofen reduce pain and swelling.
Physiotherapy. Strengthening shoulder muscles and working on shoulder control can increase stability. Your therapist will design a home exercise program for your shoulder.
Surgical Treatment
Surgery is often necessary to repair torn or stretched ligaments so that they are better able to hold the shoulder joint in place.
Arthroscopy
Soft tissues in the shoulder can be repaired using tiny instruments and small incisions. This is a same-day or outpatient procedure. Arthroscopy is a minimally invasive surgery. Your surgeon will look inside the shoulder with a tiny camera and perform the surgery with special pencil-thin instruments.
Open Surgery
Some patients may need an open surgical procedure. This involves making a larger incision over the shoulder and performing the repair under direct visualization.
Rehabilitation
After surgery, your shoulder may be immobilized temporarily with a sling.
When the sling is removed, exercises to rehabilitate the ligaments will be started. These will improve the range of motion in your shoulder and prevent scarring as the ligaments heal. Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan.
Bony Block (Please see video below)
Transfer of a bony block; either from the pelvis or through an osteotomy of the coracoid (the anterior process of the shoulder Blade). This will enable us to restore the stability of the shoulder process.
Be sure to follow your doctor’s treatment plan. Although it is a slow process, your commitment to physical therapy is the most important factor in returning to all the activities you enjoy.
Bankart Repair (Please review the video below)
The operation involves reattachment and tightening of the torn labrum and ligaments of the shoulder (see pictures below). This is usually done using sutures and small bone anchors.
The glenohumeral joint provides 60% of shoulder motion. It is a modified ‘ball and socket joint’. The humeral head moves in a complex manner over the glenoid with a combination of rolling, gliding and sliding actions.
The labrum and capsule around its rim (similar to a meniscus). The labrum is wedge-shaped and attaches almost completely around the edge of the glenoid. This creates a deeper cup for the glenoid socket. This is important because the glenoid socket is so flat and shallow that the ball of the humerus does not fit tightly. The labrum creates a deeper cup for ball of the humerus to fit into. This makes a contribution to the stability of the joint.
Remplissage Procedure
‘Remplissage’ is French for ‘to fill in’.
The procedure was described in 2007 by Wolf et al as an adjunct to the arthroscopic stabilisation procedure of the shoulder in order to address a large engaging Hill-Sach’s defect. The Remplissage technique has been reported to be effective in reducing the incidence of recurrent anterior shoulder instability when used along with arthroscopic bankart repair.
Advantages of the Remplissage technique include the ability to make the Hill-Sach’s defect extra-articular, thereby eliminating engagement of the defect with the anterior glenoid rim. It is ideally suited to instability patients who have large, engaging Hill-Sachs lesions and soft-tissue Bankart tears. These patients are known to have a higher failure rate after surgery than those with smaller lesions. The results of this technique in this difficult subset of traumatic anterior shoulder instability patients are significantly better (5% recurrence rate) than with an arthroscopic Bankart repair alone
This technique is performed when the Hill-Sachs lesion is very large and ‘engaging’ the anterior glenoid with little overhead movement (i.e. dislocating very easily due to the large Hill-Sachs lesion, as well as the Bankart lesion). In these situations, a Bankart repair alone may not be sufficient. Thus the development of the remplissage technique.
We have been performing the Remplissage procedure since 2007 and use the technique after addressing the Bankart lesion. No extra incisions (portals) are made. The arthroscope is placed through the anterior portal to view the Hill-Sach’s lesion on the back of the humeral head. Through the posterior portal, a burr is introduced to decorticate the Hill-Sach’s lesion. A triple-loaded large rotator cuff anchor is inserted into the Hill-Sach’s defect through the posterior portal. Sutures are passed through the infraspinatus tendon and the posterior capsule, which are then tied down with a ‘parachute technique’, hence successfully filling the defect on the humeral head.