Shoulder Arthritis
Normal Shoulder

In the normal shoulder (glenohumeral joint), motion occurs across smooth surfaces lined with cartilage. As seen on the X-ray to the right, the normal shoulder has smooth surfaces lined with cartilage that cushions the impact between the bones and provides a smooth gliding surface for movement.

The smooth cartilage surfaces of a normal shoulder can be seen clearly on the arthroscopic picture seen on the left.
Arthritic Shoulder
Arthritis of the shoulder develops as cartilage is broken down. This results in a loss of the smooth surfaces of the joint. The joint space seen on X-ray decreases until bone is moving on bone. Bone spurs may develop during this process. The irregular surfaces of an arthritic shoulder can be seen clearly on the arthroscopic picture seen on the right.
Osteoarthritis is a progressive degeneration of the joints. It results when the protective surface (cartilage) that allows the joint to move smoothly is damaged. Over time this cartilage is worn away, and adjacent bones are remodelled as the joint becomes increasingly abnormal and ‘rusty’, resulting in pain and stiffness.
The term osteoarthritis is derived from the three Greek words meaning bone, joint and inflammation. Traditionally thought of as a disease of progressive ‘wear and tear’, its key pathological changes of local loss of cartilage, bone remodeling and osteophyte formation instead support the view that it is a dynamic repair process gone wrong. These structural changes can significantly affect a patient’s quality of life. The common picture of arthritis of the shoulder is one of pain and stiffness and so of decreased capacity. Osteoarthritis of the shoulder is less common than many other joints, principally the hips, knees, and hands. It is nonetheless a debilitating problem and can have a significant impact on the patient’s life.
Incidence
• increases with age- more likely in patients over 60
• Demographics: more common in women
• Risk factors: 56% of patients who had primary anterior dislocation have arthrosis at 25 years follow up.
Causes
Traditionally thought of as a ‘wear and tear’ phenomenon, the cause of osteoarthritis is generally unknown; however, several contributing factors have been identified. It can be primary osteoarthritis. It can be secondary to trauma, dislocation, inflammatory/crystalline arthritis, avascular necrosis, rotator cuff arthropathy, prior shoulder surgery, history of trauma, and shoulder overuse—individuals who engage in high-intensity overhead activities such as weightlifters and racquet sport players are at increased risk.
Symptoms
Patients with arthritis of the shoulder will classically complain of a stiff and painful shoulder, with a limited range of movement. Description of pain and stiffness that intensifies with use is standard as is painful interruption of sleep. “Catching” and “noise” heard during movement is another routine finding.
Presentation
Shoulder pain
◦ worse with activities involving shoulder motion
◦ often no pain at rest
◦ Loss of range of motion
◦ especially external rotation due to anterior capsule contraction
◦ difficulty sleeping
Functional limitations at glenohumeral joint
◦ decreased range of motion
◦ variable and more active patients have better range of motion (ROM)
◦ crepitus
◦ catching/squeaking with articulation
Symptoms
Pain. The most common symptom of arthritis of the shoulder is pain. This pain is aggravated by activity and progressively gets worse over time. The location of the pain will vary, depending on which shoulder joint is affected:
- If the glenohumeral shoulder joint is affected, the pain is centered in the side or back of the shoulder and may intensify with changes in the weather. Patients complain of an ache deep in the joint.
- The pain of arthritis in the acromioclavicular (AC) joint is focused on the top of the shoulder. This pain can sometimes radiate or travel to the side of the neck.
- Someone with rheumatoid arthritis may have pain throughout the shoulder if both the glenohumeral and AC joints are affected.
As th disease progresses, any movement of the shoulder causes pain. Night pain is common, and sleeping may be difficult.
Other symptoms may include:
Limited range of motion. Limited motion is another common symptom. It may become more difficult to lift your arm to comb your hair or reach up to a shelf.
Crepitus. You may hear a grinding, clicking, or snapping sound (crepitus) as you move your shoulder. Crepitus is sometimes painful and can be loud enough for other people to hear,
Diagnosis
Osteoarthritis is usually diagnosed by a combination of clinical examination and history of the presenting complaint. Before proceeding with treatment, X-rays may be taken to evaluate the extent of any damage which may help decide upon the most appropriate treatment. Similarly, a CT scan of the shoulder may also be requested if it is decided that surgical management would be the most suitable option.
Treatment
Non-surgical Management
As with other arthritic conditions, initial treatment of arthritis of the shoulder is nonsurgical. Prof Imam may recommend the following:
- Rest or change in activities. You may need to change the way you move your arm to avoid provoking pain.
- Physical therapy exercises may improve the range of motion in your shoulder.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, or naproxen, may reduce inflammation and pain. These medications can irritate the stomach lining and cause internal bleeding. They should be taken with food. Consult with your doctor before taking over-the-counter NSAIDs if you have a history of ulcers or are taking blood thinning medication.
- Corticosteroid injections in the shoulder can dramatically reduce the inflammation and pain. However, the effect is often temporary.
- Moist heat may provide temporary relief.
- Icing your shoulder for 20 to 30 minutes two or three times a day to reduce inflammation and ease pain.
- If you have rheumatoid arthritis, your doctor (typically a rheumatologist) may prescribe a disease-modifying drug, such as methotrexate.
- Dietary supplements, such as glucosamine and chondroitin sulfate may help relieve pain. (Note: There is little scientific evidence to support the use of glucosamine and chondroitin sulfate to treat arthritis. In addition, the U.S. Food and Drug Administration does not test dietary supplements. These compounds may cause negative interactions with other medications. Always consult your doctor before taking dietary supplements.)
Surgical Management
The form of surgery chosen should be the least invasive approach required to provide long term pain relief and restore function.
Arthroscopic Treatment
Arthroscopic treatment of the shoulder for osteoarthritis is primarily a temporary therapy in which the joint is “tidied up.” The surgeon removes unwanted material and smoothes off the joint, hopefully providing relief of symptoms.
Shoulder Replacement
Non-operative Management
Non-operative treatment should always be exhausted prior to proceeding with any form of surgery.
Ultimately in cases of severe non-resolvable pain or previously failed treatment options, shoulder replacement (arthroplasty) is indicated. There are several variations of shoulder replacements available, some more invasive than others. The choice of replacement depends on several criteria. These include age, activity level, a form of arthritis, and the amount of bone affected.
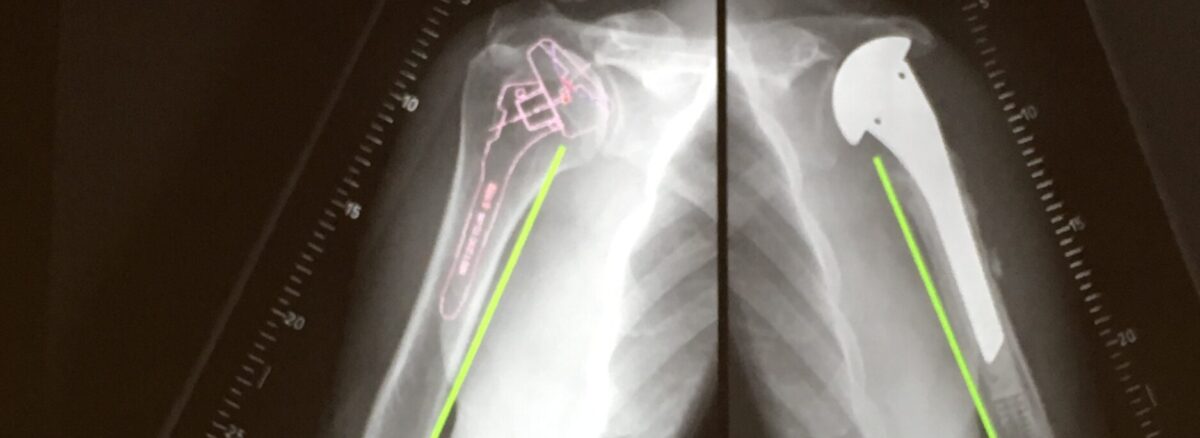
Arthroplasty Options
Hemiarthroplasty
Hemiarthroplasty involves a prosthetic metal implant being placed into the upper bone in the arm (humerus) which forms half of the shoulder joint. Whilst in total shoulder arthroplasty both sides of the joint are replaced. Depending on the condition of your shoulder, your surgeon may replace only the ball. This procedure is called a hemiarthroplasty. In a traditional hemiarthroplasty, the head of the humerus is replaced with a metal ball and stem, similar to the component used in a total shoulder replacement. This is called a stemmed hemiarthroplasty.
Resurfacing Hemiarthroplasty
Resurfacing hemiarthroplasty involves replacing just the joint surface of the humeral head with a cap-like prosthesis without a stem. With its bone preserving advantage, it offers those with arthritis of the shoulder an alternative to the standard stemmed shoulder replacement.
Total Shoulder replacement
The typical total shoulder replacement involves replacing the arthritic joint surfaces with a highly polished metal ball attached to a stem and a plastic socket. Patients with bone-on-bone osteoarthritis and intact rotator cuff tendons are generally good candidates for conventional total shoulder replacement.
Reverse Shoulder Replacement
Another type of shoulder replacement is called reverse total shoulder replacement. Reverse total shoulder replacement is used for people who have:
• Completely torn rotator cuffs with severe arm weakness
• The effects of severe arthritis and rotator cuff tearing (cuff tear arthropathy)
• had a previous shoulder replacement that failed
Reverse shoulder replacement is a type of shoulder replacement in which the glenohumeral joint’s normal ball and socket relationship is reversed, creating a more stable joint with a fixed fulcrum. This form of shoulder replacement is utilized in situations where conventional shoulder replacement surgery leads to poor outcomes and high failure rates. The combination of improved design features and excellent clinical outcome data has led to reverse shoulder replacement instead of other types to primary manage various shoulder problems. We have published our results as part of a multicentre clinical study looking at 159 reverse shoulder replacement results with five years of follow-up. We reported that reverse total shoulder arthroplasty restores the function in the shoulder with significant improvements in function and moderate complications with significant improvement in clinical functions.
Prevention
- Keep doing as much of your regular routine as possible.
- Maintain a healthy weight
- Remain active to keep muscle strength from diminishing. If you work up to a well-designed exercise program, you can keep or even improve joint flexibility.
- Keep repetitive overhead activity to a minimum
- Rest only when joints are very painfulCan you play sport with shoulder arthritis?
Arthritis and Sports
By managing pain and symptoms, many people with osteoarthritis can continue to exercise and enjoy sports. Seeking treatment early can help.
To avoid pain, people sometimes stop exercising.
But it doesn’t have to be that way.
High-impact sports and repetitive motions can contribute to arthritis, but patients should not be afraid of exercise. Research has shown that even running did not increase osteoarthritis among individuals who were already runners.
The key is to be active all week. Weekend warriors are more prone to injury.
The key is to be active all week, explains Dr. Kohler. Weekend warriors who go all-out on Saturday and Sunday, but have desk jobs and do minimal activity during the week, are more prone to injury. This also places them at risk for osteoarthritis. Studies have shown that even five or 10 minutes of exercise slipped into the weekday can help, she says.
“If you’re able to stay active on a more regular basis, then your body is more conditioned to keep up with the activities you want to do,” Dr. Kohler says. “Aging tendons are less pliable so incorporating stretching is also important.”
Exercise keeps bone density high, lowering fracture risks, and muscles conditioned, which reduces the risk of falls. “Staying physically active can also potentially reduce inflammation, which contributes to osteoarthritis,” Dr. Kohler says. “That’s why we always talk about exercise as the best medicine.”
Tips for Staying Active:
- Exercise a few times a week, even if only for five to 10 minutes.
- Stretch before exercise.
- Be aware of your anatomy, weight, past injuries and family history, which can be osteoarthritis risk factors.
- Arthritis-like symptoms in your 20s require medical evaluation. It could be a sign of an
- autoimmune disease.
- Try the Mediterranean or anti-inflammatory diets to improve osteoarthritis symptoms.
- Avoid sugar and red meat, which can increase inflammation.
When You Have Pain:
- Treat a sprain or injured tendon by stopping activity temporarily.
- Try over-the-counter non-steroidal anti-inflammatory medicine to reduce swelling.
- After exercise, use ice, if you have swelling and know you overdid it. If you know the area swells or is stiff often, use heat.
- Gradually return to exercise, even if the swelling is down. Immediate aggressive exercise after injury can risk further injury.
- When you have pain, swelling and warmth in the joint region or persistent pain, see a doctor.