Innovative Tendon Transfer Solutions for Irreparable Rotator Cuff Tears
Introduction:
Welcome to our online platform, the arm doc, where we discuss options for patients with Massive, Irreparable Posterior Superior Rotator Cuff Tears (RCTs). This condition, often accompanied by pseudo-paralysis and atrophy of the Teres Minor, poses significant challenges, especially for young patients with severely limited shoulder function.

Massive irreparable tears render the rotator cuff tendons degenerated and beyond traditional repair. Diagnostic tools such as MRI scans reveal the extent of irreparability, showcasing completely wasted rotator cuff tendons.
MRI scan showing irreparable (completely wasted rotator cuff tendon)
A view in the shoulder during key hole surgery showing absent rotator cuff tendons 
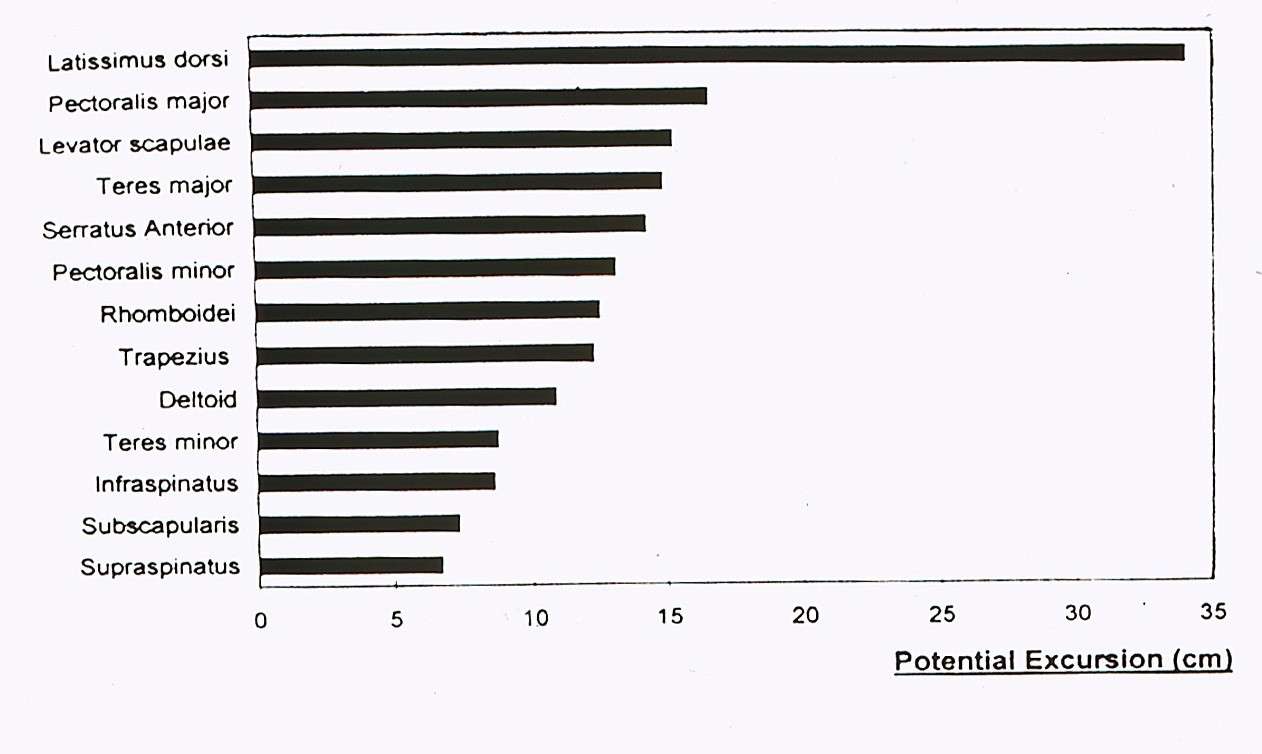
To address this issue, we explore innovative tendon transfer options, including:
- Latissimus Dorsi Tendon
- Teres Major Tendon
- Lower Trapezius Tendon
- Latissimus dorsi tendon

- Teres Major Tendon

- Lower Trapezius tendon

Our Preferred Solution: Lower Trapezius Tendon Transfer
Our tendon transfer of choice is the Lower Trapezius Tendon, a technique originally popularised by Professor Bassem El Hassan from Harvard. This preference is based on several key factors:
- Long-term outcomes
- Achievement of better function
- Alignment with the natural line of pull of the rotator cuff tendons, as confirmed through cadaveric lab dissection
- Similar length and strength to the original tendons
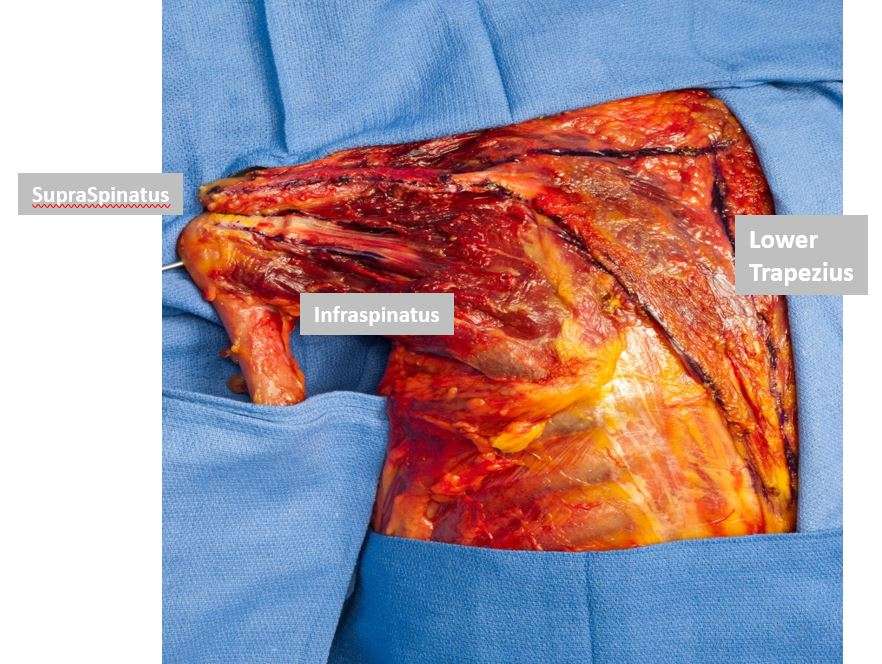
This tendon has a similar length and strength to the original tendons
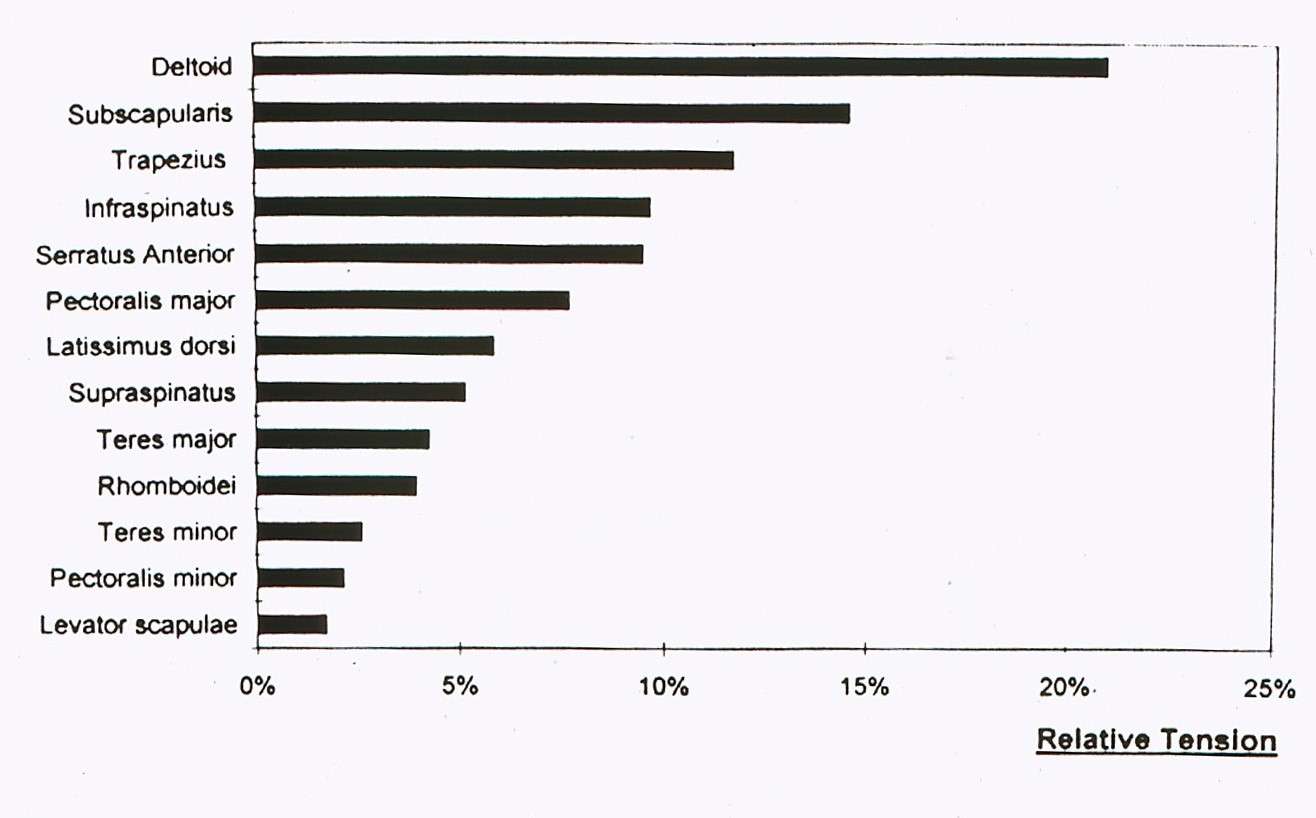
So, to summarise, anatomically, Kinematically, and biomechanically, this is the Best Transfer to Reconstruct Posterior-Superior irreparable rotator cuff tears.
Contraindications:
Tendon transfers may not be suitable for elderly patients with reduced activity levels, those with advanced arthritis, or individuals with unstable shoulders. In such cases, a reverse shoulder replacement is a more appropriate alternative.
In these patients, a reverse shoulder replacement would be a better option. 
Surgical Considerations:
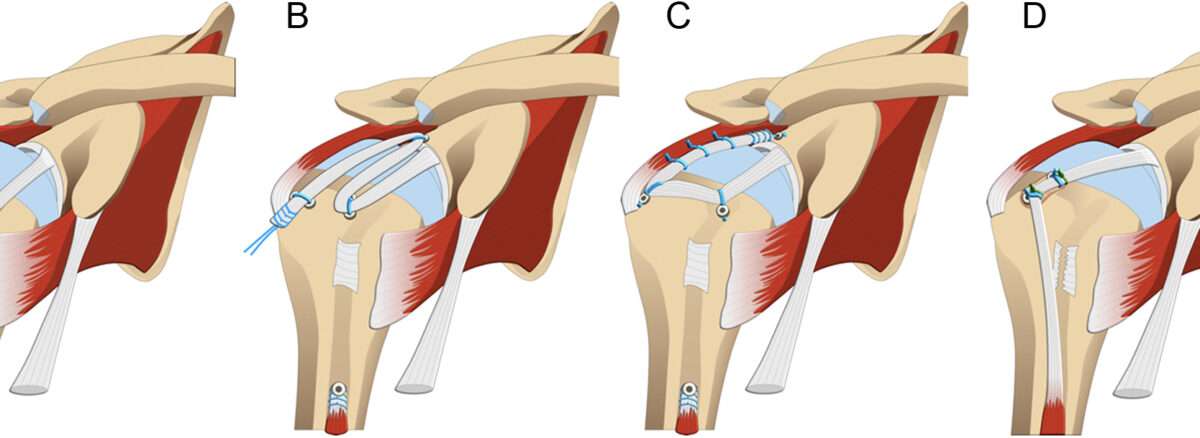
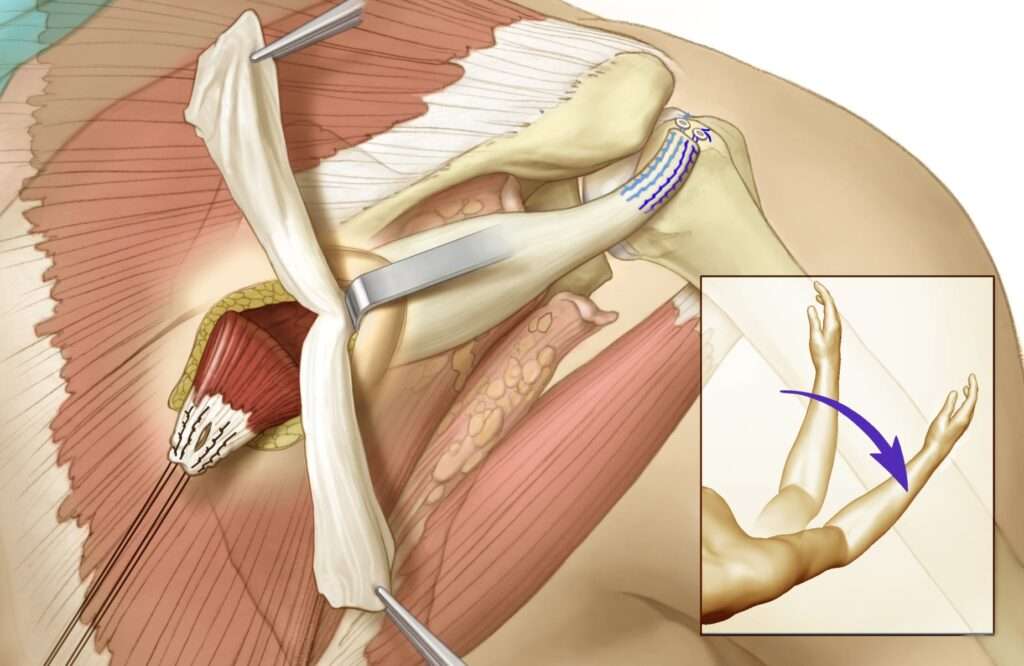
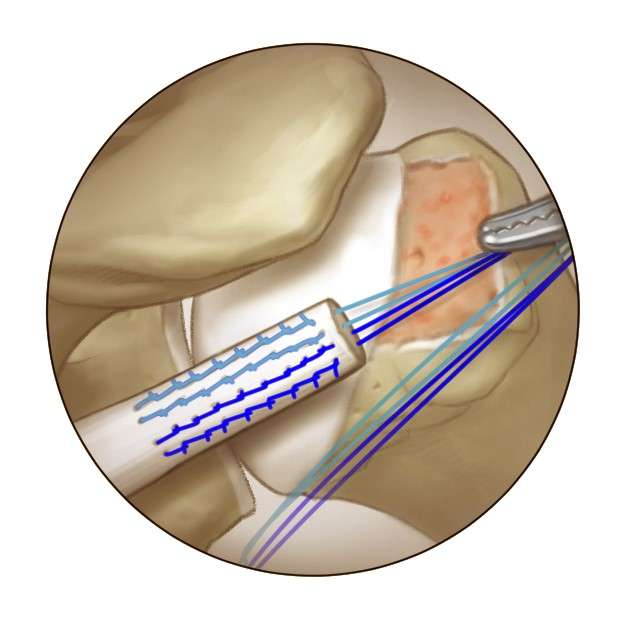
For eligible patients, the surgical procedure is conducted through an arthroscopic-assisted technique. The patient is positioned sitting, and the Lower Trapezius Tendon is marked on the back of the shoulder. An incision is made to harvest the tendon, and an Achilles tendon graft from a cadaver is utilized to augment the transfer. The Achilles tendon is then connected to the top of the arm bone in the shoulder, ensuring optimal function.
The Surgical Technique in Summary:
- Arthroscopic-assisted procedure
- Surgery performed in the sitting position
- Identification and harvesting of the Lower Trapezius Tendon
- Augmentation with an Achilles tendon graft
- The surgery is done in the sitting position.

- The lower trapezius tendon is marked on the back of your shoulder

- The incision is marked on the back of your shoulder to harvest the lower trapezius tendon

- An Achilles tendon graft is retrieved from a cadaver to augment the transfer.

- The Achilles tendon is attached to the top of your arm bone in the shoulder.
Post-Surgery Rehabilitation:
A comprehensive physiotherapy protocol is essential for restoring function after the procedure.
Rehabilitation Protocol
Lower Trapezius Tendon Transfer to Greater Tuberosity
PHASE I: Protected ROM (8 weeks)
- Patients may shower immediately over clear plastic, waterproof dressing
- Sutures are all underneath the skin and will dissolve on their own
- Ice or cold flow systems are encouraged for the first week at a minimum: should be used 3-4 times per day.
- Gunslinger brace should be in place when not performing exercises.
- Avoid all active and active assistive exercises until cleared by the surgeon. This includes pulley exercises, wand and supine-assisted exercises.
- Initiate exercise program three times per day:
- Immediate elbow, forearm and hand range of motion out of the sling
PHASE II: Progressive ROM (6 to 12 weeks)
- May discontinue brace at 6 weeks.
- Passive external rotation of the shoulder to tolerance – instruct family member (start at 6 weeks)
- PROM into scapular plane elevation to 120 degrees (start at six weeks)
- At 6 weeks, perform overhead reach (see below)
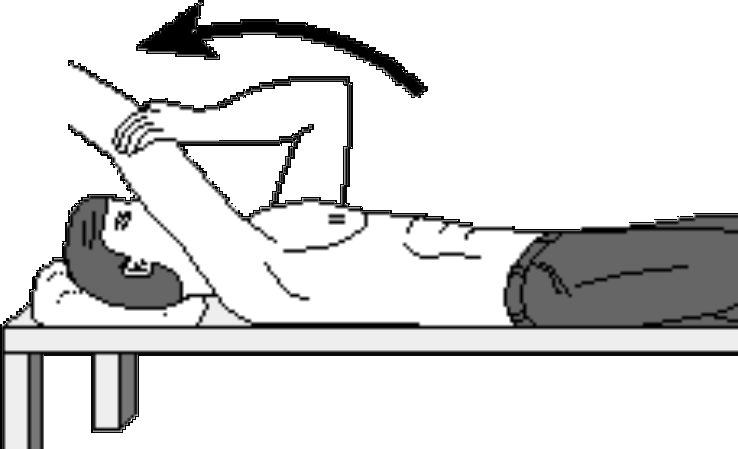
Overhead reach is helping to lift your stiff arm up as high as it will go. To stretch your overhead reach, lie flat on your back, relax, and grasp the wrist of the tight shoulder with your opposite hand. Using the power in your opposite arm, bring the stiff arm up as far as it is comfortable. Start holding it for ten seconds and then work up to where you can hold it for a count of 30. Breathe slowly and deeply while the arm is moved. Repeat this stretch ten times, trying to help the arm up a little higher each time.
- May start active scapular mobility exercises at 6 weeks – Must keep the shoulder musculature relaxed.
- Start AAROM and AROM – includes pulleys, wand and supine gravity-assisted exercises at 8 weeks. Emphasise all motions except IR behind the back and cross-body adduction until three months.
- Isolate and strengthen scapular stabilisers.
- Progress PROM and capsular stretching of the shoulder as needed – elevation and external rotation as tolerated
- Avoid resisted training or strengthening. Avoid AROM in positions of subacromial impingement.
PHASE III: (> 12 weeks)
- The lifting restriction of 5 pounds should be reinforced with the patient.
- Start progressive rotator cuff and shoulder strengthening at 3 months –isometrics initially.
- Initiate isotonic strengthening at 4-5 months (Theraband, dumbbells, Hughston’s exercises, etc). Include a home cuff strengthening program. Continue to emphasise scapular stabilisers.
- Equate active and passive range of motion. Encourage scapulohumeral mechanics during active shoulder motion.
- Simulate work/recreational activities as rotator cuff strength and endurance improve.
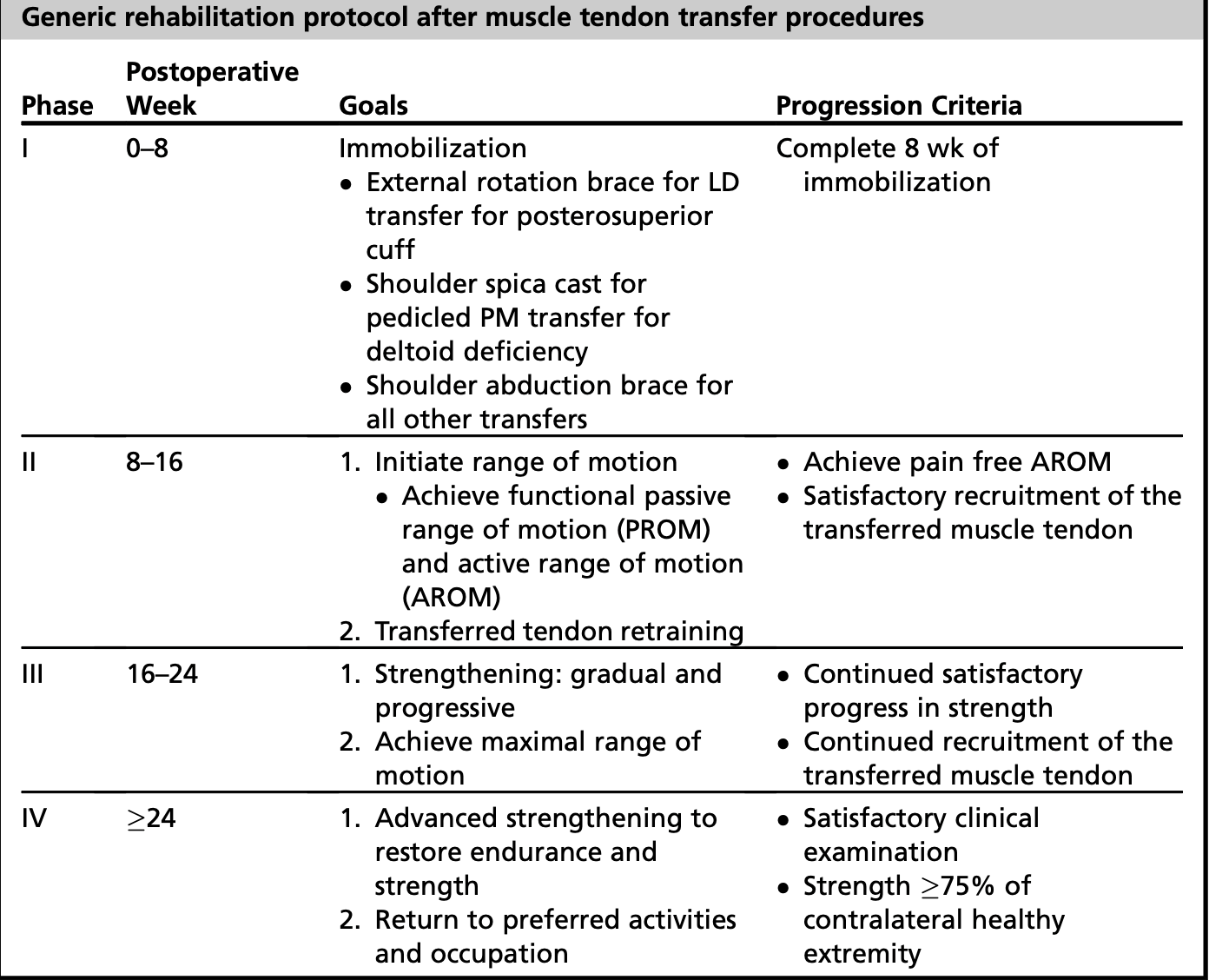
The full function can be anticipated after the completion of the physiotherapy protocol.
VIDEO
Evidence
Evidence supports this innovative approach from a study involving 16 patients with prior Superior Capsular Reconstruction (SCR). The average age was 49 years, with 15 males and 1 female. Indications for surgery included persistent symptoms, particularly weakness in external rotation and flexion after SCR. At an average follow-up of 29 months, 15 patients demonstrated significant improvement in all scores, with the most notable improvement seen in external rotation—from -20 to +30 degrees.