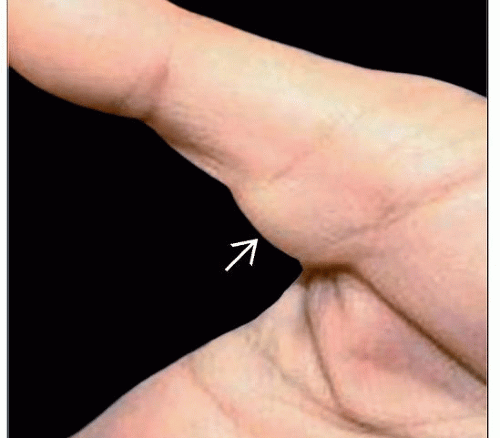
Giant Cell Tumor of Tendon Sheath
It is a common finding which is usually benign. The second most common soft-tissue tumour seen in the hand, following ganglion cyst. Chassaignac first described these benign soft-tissue masses in 1852, and he overstated their biologic potential in referring to them as cancers of the tendon sheath.
- Common in patients aged 30-50 years old
- Anatomic location
Presentation
Signs & Symptoms
- enlarging mass
- pain, worse with activity (or wearing shoes, for foot lesions)
- firm, nodular mass that does not transilluminate
The symptoms of these masses depend on which subtype you have. Some possible symptoms include the following:
Imaging
- Plain radiographs
- To help show the status of the bone underneath
- Ultrasound
able to demonstrate the relationship of the lesion with adjacent tendon - most have some internal vascularity
- MRI
- MRI may be helpful diagnostically
Other causes to consider?
- Ganglion cyst
- cystic component
- Pigmented villonodular synovitis (PVNS)
- histologically identical
- involves larger joints
- Desmoid tumour
- fibroma/fibrosarcoma
- glomangioma
Treatment
Surgery
Surgery is the main treatment for tenosynovial giant cell tumors. Your doctor may remove some or all of the tumors, as well as the inflamed joint tissue. You may need another surgery if the tumorreturns.
Surgical procedure:
- marginal excision
- High recurrence rate
- more common if tumour extends into joints and deep to the volar plate
- tendon involvement is associated with a high recurrence rate
- local recurrence is usually treated with repeat excision
- the operative approach is dependent on the location and extent of the tumour
For Professionals
The incidence of local recurrence is high, ranging from 9% to 44%. Researchers have reported the following rates:
The variability in rates probably reflects incomplete excision of the lesions, especially the satellite nodules. Risk factors for recurrence include the following: