DeQuervain’s Disease
De Quervain’s tendinosis occurs when the tendons around the base of the thumb are irritated or constricted. The word “tendinosis” refers to a swelling of the tendons. Swelling of the tendons, and the tendon sheath, can cause pain and tenderness along the thumb side of the wrist. This is particularly noticeable when forming a fist, grasping or gripping something, or when turning the wrist.
Other names
– DeQuervain’s tenosynovitis
– First extensor compartment tenosynovitis
Who does it affect?
Usually adults, slightly more common in females.
Why does it occur?
Two of the main tendons to the thumb pass through a tunnel (or series of pulleys) located on the thumb side of the wrist. Tendons are rope-like structures that attach muscle to bone. Tendons are covered by a slippery thin soft-tissue layer, called synovium. This layer allows the tendons to slide easily through a fibrous tunnel called a sheath.
Any swelling of the tendons and/or thickening of the sheath results in increased friction and pain with certain thumb and wrist movements.
The tendons on the back of the wrist travel through separate tunnels at the wrist joint level. These tunnels are to ensure that the tendons do not bowstring when the wrist is extended (cocked back). The space inside the tunnel is lubricated but limited.
If inflammation occurs in the tunnel, then the tendons may become irritated, and friction between the tendon and tunnel roof may occur. This would cause pain and swell inside the tunnel. DeQuervain’s disease is inflammation of the tendons in the first extensor compartment. This compartment is on the back of the wrist (not the palm side) at the base of the thumb.
De Quervain’s tendinosis may be caused by overuse. It also is associated with pregnancy and rheumatoid disease. It is most common in middle-aged women.
Symptoms
• Pain may be felt over the thumb side of the wrist. This is the main symptom. The pain may appear either gradually or suddenly. Pain is felt in the wrist and can travel up the forearm. The pain is usually worse when the hand and thumb are in use. This is especially true when forcefully grasping objects or twisting the wrist.
• Swelling may be seen over the thumb side of the wrist. This swelling may accompany a fluid-filled cyst in this region.
• A “catching” or “snapping” sensation may be felt when moving the thumb.
• Pain and swelling may make it difficult to move the thumb and wrist.
• This may be accompanied by a palpable and sometimes audible “creaking” sensation.
Clinical Examination
Investigations
The diagnosis of De Quervain’s is often very clear from the history and clinical examination. In such cases, no special tests are required.
`ÛHowever, an ultrasound scan can visualise the tendons and look for abnormal fluid, thickening and inflammation.
What is the prognosis of De Quervain syndrome?
The outlook for this condition is good, unless you neglect it. In this case, you could suffer from trapeziometacarpal osteoarthritis, which is a type of arthritis affecting the base of the thumb.
How can De Quervain syndrome be prevented?
This condition can be prevented by changing your habits and paying more attention to the onset of the inflammation.
Non-operative treatment
A resting splint and physiotherapy can often help early cases of De Quervain’s.

A low dose corticosteroid injection into the sheath may lubricate and also damp down the inflammation. Steroid injections are not often repeated.
Further attempts may damage the skin and dissolve fat leaving the tendons very prominent and the skin pigmentation altered.
Therefore surgery would be advised after one or two failed injections.
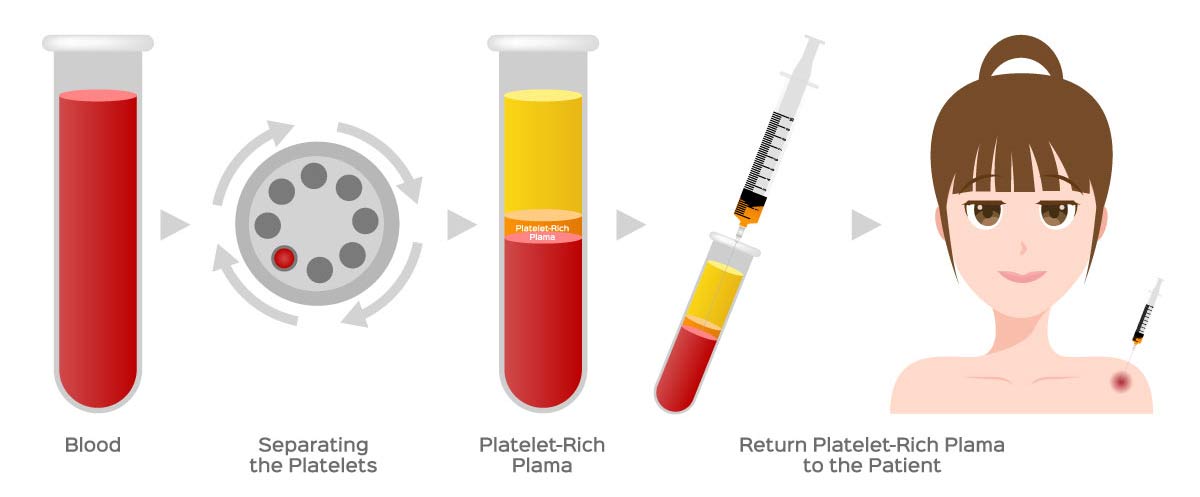
There is evidence supporting the use of Platelet-rich plasma.
Operative treatment
The surgery is a day case procedure usually under local or General anaesthetic and takes about 10 minutes.
A tourniquet is not often used, like adrenaline ( a vasoconstrictor) is mixed with the local anaesthetic to reduce bleeding.
The surgery is performed through a 2cm transverse skin crease incision. Local anaesthetic (with adrenaline) is infiltrated under the skin in line with the incision at the thumb side of the wrist. Once numb, the skin is incised, and the underlying fat is retracted. Care is taken not to injure sensitive nerves and blood vessels. At the base of the wound is the extensor compartment sheath.
This structure needs to be released to allow the tendon and its nodule to glide in and out without catching. Occasionally multiple small sub-compartments need to be released. The skin is sutured with absorbable stitches under the skin ( no need to be removed), and a bulky dressing is applied.
Post-operative rehabilitation
The patient is fit to go home soon after the operation. The anaesthetic will wear off after approximately 6 hours. Simple analgesia usually controls the pain and should be started before the anaesthetic has worn off. The hand should be elevated as much as possible for the first five days to prevent the hand and fingers from swelling. Gently bend and straighten the fingers from day one.
My preference is to remove the dressing for two days.
The wound is cleaned and redressed with a simple dressing.
Avoid forced gripping or lifting heavy objects for 2-3 weeks.
The sutures dissolve at about 2-3 weeks.
You should notice an improvement in symptoms within a few days, but the final result may be realised at about three months.
Return to activities of daily living
It is my advice to keep the wound covered and dry until the wound has healed at 7-10 days.
Return to driving:
The hand needs to have full control of the steering wheel and left hand the gear stick and be able to control the vehicle in an emergency. It is probably advisable to delay returning to driving for a few days if the hand is tender. However, everyone is different, and some people feel able to drive straight away after the operation.
Return to work:
Everyone has different work environments.
Light desk-based activities can be performed immediately.
Returning to heavy manual labour should be prevented for approximately 4 – 6 weeks. Early return to heavy work may cause the tendons and nerve to scar into the released ligament. Please ask your surgeon for advice on this.
Complications
Overall greater than 95% are happy with the result. However, complications can occur.
There are complications specific to DeQuervain’s disease and also general complications associated with hand surgery.
Please look at my general hand complications page by clicking here but also see below for some specific complications.
Specific complications:
Failure to completely resolve the symptoms (approximately 1% – this may be due to failure to completely release all the tendon sub sheaths. This should be rare but may be released again).
The nerves just under the skin are notoriously sensitive; if damaged, a painful neuroma can develop. Extra care is taken with these nerves to keep this risk to a minimum.


