Base of thumb arthritis
Background
Arthritis is a condition that irritates or destroys a joint. Although there are several types of arthritis, the one that most often affects the joint at the base of the thumb (the basal joint) is osteoarthritis (degenerative or “wear-and-tear” arthritis).
Also known as
– Basilar thumb OA
– Thumb Carpo-metacarpal joint OA (CMCJ OA)
– Thumb Trapezio-metacarpal joint OA (TMCJ OA)
– Saddle joint OA
Who does it affect?
Arthritis of the base of the thumb is more common in women than in men, and usually occurs after 40 years of age. Prior fractures or other injuries to the joint may increase the likelihood of developing this condition.
Nearly 40% of post-menopausal women have radiographic changes at the base of the thumb, 10% seek medical treatment, and 1% are severely afflicted.
The base of thumb OA is more common in females than males and is usually starts over 50 years of age. Usually as a result of a previous fracture.
Why does it occur?
It is caused by the loss of cartilage inside the thumb joint due to wear and tear. Genetics are also believed to play a key part in the development of the condition.
We use our thumbs continually throughout our waking lives and the loss of cartilage, which acts as a cushion inside the joint, can cause bone to rub against bone, resulting in severe pain and loss of function. Women are six times more likely than men to develop thumb arthritis.
There are two types of OA. Primary and Secondary. Primary OA is the most common cause and is simple wear and tear. Abnormal loads across the joint cause the articular cartilage (slippy ends of bones) to wear away, leaving bone on the bone ends rubbing together.
Secondary OA often occurs after a fracture into the joint, causing a sharp bone surface to rub and wear the joint away.
Symptoms
⦁ Pain with activities that involve gripping or pinching, such as turning a key, opening a door, or snapping your fingers
⦁ Swelling and tenderness at the base of the thumb
⦁ An aching discomfort after prolonged use
⦁ Loss of strength in gripping or pinching activities
⦁ An enlarged, “out-of-joint” appearance
⦁ Development of a bony prominence or bump over the joint
⦁ Limited motion
Clinical Examination
Bony swelling is apparent at the base of the thumb in more advanced cases, and local palpation at the base of the thumb is tender.
Specific tests include the Axial Grind Test, whereby the thumb is pushed along its long axis towards the base of the thumb. The reduction Relocation test involves pressing the base of the thumb joint with one hand whilst circumducting the end of the thumb with the other hand.
Investigations
X-rays of the thumb reveal the typical loss of joint space and osteophyte (extra bone) formation.
We obtain three X-ray views: a thumb CMCJ AP (Robert View) and an AP and Lateral Wrist. The lateral wrist helps me look at the alignment of the wrist bones and, in particular, the lunate bone to ensure no co-existing ligament attenuation in the wrist. The Robert view is the best view to see the joint and notice the abnormal surfaces.
Non-operative treatment
– Rest, pain killers (analgesia) and avoidance of provoking activities.
– Resting night splint prescribed by a hand therapist
– Intra-articular steroid injection.
Most patients have joints that are easy to palpate, and we inject them in the clinic. However, the other half are more difficult and require the injection to be performed under X-ray control. We prefer only perform one or two injections before considering surgery. The risks associated with steroid injection are small. Still, they include failure to give long-lasting benefit and a small risk of causing a skin reaction with altered skin pigmentation or, in severe cases thinning of the fat under the skin.
Operative treatment
If non-operative techniques have been tried and have not given long-lasting benefits, some patients may elect to undergo surgery.
Surgery aims to prevent the two ends of the bone from rubbing against each other.
I would always discuss the options available, and the patients’ age and functional demands may guide these.
The main options are :
⦁ Thumb resurfacing procedure
⦁ Trapeziectomy – remove the trapezium bone and allow the space to fill with scar tissue
⦁ Thumb CMCJ Fusion – fuse the trapezium and thumb metacarpal bones to make a solid joint
⦁ Thumb CMCJ replacement – remove the ends of the bone and insert a new artificial joint replacement.
The decision about which particular surgery is the most appropriate for an individual patient is made considering the patient’s functional demands and the preoperative X-ray.
Surgery is performed under general anaesthetic or regional anaesthesia (only the arm is made numb). Each of the surgeries listed above takes less than an hour.
The skin is sutured with absorbable buried stitches and immobilised with a half Plaster of Paris slab applied.
Trapeziectomy
In the past, having removed the trapezium, I used to perform ligament reconstructions, fill the space with rolled up tendon or perform a sling-type procedure. However, having studied the literature, I now simply remove the trapezium and repair the joint capsule. The left space seems to fill with scar tissue, and the results in my practice tho no difference over the more involved sling/reconstruction type procedures.
What is a trapeziectomy?
Osteoarthritis can occur in the trapezium, which is the cube-shaped bone in your wrist that is joined to the base of your thumb (the trapeziometacarpal joint). This can be a very painful condition, causing pain when you use your thumb and limiting you from normal activities.
A trapeziectomy is a surgical procedure that is used to relieve pain and to enable the thumb joint to work as it should.
What are the risks of a trapeziectomy?
The possible complications of the procedure may include:
⦁ Continued feelings of numbness in the thumb
⦁ Damage to the artery that passes near to the trapezium
⦁ Severe pain and stiffness
What can I expect during recovery?
Following the procedure, you should be able to go home on the same day. You will be instructed to keep your hand raised for two weeks. After four to six weeks, your bandage will be removed. Over the course of the next few years, your thumb should continue to get back to a good range of movement with the help of regular exercise.
One of the main risks of trapeziectomy is proximal migration of the thumb metacarpal. If this occurs, it can be very difficult to stabilise the thumb and ultimately may require a procedure to fuse the thumb metacarpal to the index metacarpal, which is difficult. Proximal migration would be a major concern in a younger individual, and in such cases, most people would prefer a thumb CMCJ fusion or a total joint replacement.
Another procedure that we tend to do is mini-tight rope. This restores the stability of the first CMC joint.
This is Prof Imam’s preferred trapeziectomy procedure.
Trapeziectomy and mini tight rope
See Video Below
CMC Suspensionplasty with tendon Graft and InternalBrace Ligament Augmentation
See Video below.
Cartiva CMC Resurfacing replacement
Cartiva synthetic cartilage implant surgery is performed under local anaesthetic, which means the patient is awake but sedated throughout. A 1.5 inch incision is made at the back of the thumb and a hole is drilled into the first metacarpal (thumb bone). The implant is inserted into the hole and the incision is closed with stitches.
Patients normally go home the same day and wear a bandage for around 10 days. Physiotherapy helps with rehabilitation and strengthening the thumb joint. Within three to six months of surgery, the patient will normally have the same level of strength as someone who doesn’t have thumb osteoarthritis. Full recovery can take up to a year. The procedure is suitable for anyone except patients with the most severe stage four arthritis as their joint is normally too damaged to be able to take an implant.
Thumb CMCJ fusion
We prefer a thumb CMCJ fusion in physically high demand patients, under 50 yrs of age. The ends of the bone are removed with a small saw and then brought together and held with two staples. Over the next six weeks or so, the bone grows across the joint and abolishes any movement and hence pain present at the joint.
The thumb is somewhat stiffer than normal, and patients will not be able to contour their dumb flat against a table. Most do not consider this a problem and are happy that the thumb is pain-free and strong.
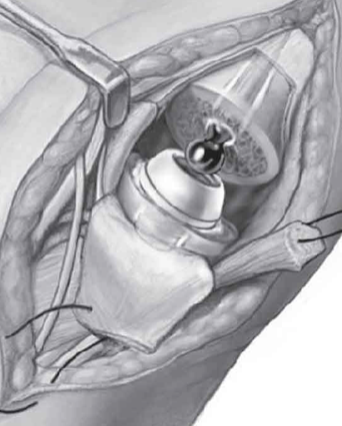
Thumb CMCJ replacement
This is a relatively new concept in the UK but very popular in Europe. The ends of the bone are removed, and a new joint is inserted, similar to a mini hip replacement. The results are very good, and I am increasingly offering this as an alternative.
Postoperative rehabilitation
The patient is fit to go home soon after the operation, usually on the same day. Simple analgesia usually controls the pain postoperatively and should be started on discharge.
The hand should be elevated as much as possible for the first five days to prevent swelling in hand and fingers. Gently bend and straighten the fingers from day 1. The back slab Plaster of Paris is removed in the first week when the wound is cleaned, redressed, and therapy made splint (cast) is applied.
The sutures are usually dissolvable and buried under the skin. The splint (cast) is kept for approximately 6-8 weeks. Therapy exercises will commence regaining mobility and strength. Patients usually notice that the arthritic pain has gone within eight weeks, but the results improve as the thumb strengthens between 6 and 12 months
Return to activities of daily living
The wounds should be kept covered and dry for the first 10days until the wound has healed.
The splint or cast should be kept dry, which can be gradually removed with the supervision of my hand therapist.
Return to driving: The hand needs to have full control of the steering wheel and left hand the gear stick. It is probably advisable to delay your return to driving until you are pain-free and can control a car in an emergency. This may be between 8 and 12 weeks, although everyone is different, and some patients feel safe to drive within a few weeks.
Return to work: Everyone is involved in different working environments. Return to heavy manual labour should be prevented for approximately 8weeks. Please ask your surgeon for advice on this.
Complications
Overall, greater than 85% are happy with the result. However, complications can occur.
There are complications specific to thumb surgery and also general complications associated with hand surgery.
Specific complications:
Failure to completely resolve the symptoms (this may be due to arthritis in adjacent joints, this should be rare but may require further surgery).
The thumb will be weaker on the opposite side, which should improve with time, but will never be normal.
Proximal migration of the thumb metacarpal (5%). This can occur after a trapeziectomy when the thumb metacarpal drops down into the space left once the trapezium has been removed. It can be improved using a sling-type procedure to hold up the thumb or the thumb be fused.
Non-union (5-10%). This is only relevant to a thumb CMCJ fusion when the bone ends do not join. Occasionally this is painless and can be left alone. If painful revision surgery may be needed repeating the operation using bone graft or performing a trapeziectomy
Dislocation (5% – 10% when an implant is used), occasionally, when an implant is used, there is the risk of dislocation, but the theoretical benefit is of a stronger thumb. If it dislocates, it may need to be removed and the space dealt with in other operations.